In Brief: ECG has analyzed proprietary market data and has published the most comprehensive compensation and productivity data for NES.
In a healthcare landscape marked by rising costs and increasing patient demand for safe, effective, and efficient treatment, provider organizations are seeking low-cost, low-impact treatment alternatives. Enter neuroendovascular surgery (NES).
NES is a subspecialty that uses “minimally invasive catheter-based technology, radiologic imaging, and clinical expertise to diagnose and treat diseases of the central nervous system, head, neck, and spine” and offers patients “smaller incisions, faster recovery, and less pain than traditional surgery.” As a result of these benefits, ECG has encountered more healthcare organizations recruiting for NES physicians in recent months. These entities, though located in different geographic markets across the country, are all facing the same challenge: how to accurately value NES services.
To help address this issue, ECG is conducting a rapid survey that is entirely dedicated to this subspecialty. In addition, we’ve outlined three other considerations to help your organization implement fair and competitive compensation models for these valuable services.
Consideration One: Compensation Should Reflect NES as a Subspecialty
NES is a subspecialty within the fields of neurosurgery, neurology, and radiology, meaning physicians must complete additional specialized training to supply these services. In fact, to perform NES procedures, providers must:
- Acquire an MD or DO degree with board eligibility/certification.
- Complete one of the following ACGME-accredited or -recognized programs:
- A neurosurgical residency
- A neurology residency followed by a stroke or critical care fellowship
- A radiology residency followed by a neuroradiology fellowship, during which at least six months are focused on clinical service in a neurosurgery, vascular neurology, or neurointensive care program
- Complete a 24‑month fellowship in neuroendovascular intervention in an approved fellowship program.
Moreover, since NES is also referred to as neurointerventional surgery, endovascular surgical neuroradiology, and interventional neuroradiology, there is no specific data for the subspecialty. Organizations should ensure compensation accounts for the services being provided, because published neurosurgery, neurology, or radiology benchmark data may not appropriately reflect NES as its own subspecialty.
Consideration Two: Provider Recruitment Is a Critical Issue Impacting Staffing and Reimbursement
Organizations looking to appropriately value NES services must recognize—and account for—a highly competitive recruitment environment. Across all specialties, the US is projected to have a shortage of 81,180 full-time equivalent physicians by 2035. Neurosurgery and radiology have some of the lowest supply adequacies at 89% each. And while estimates for NES were unavailable, in ECG’s experience, provider demand is equal to or greater than the supply of neurosurgeons, neurologists, and radiologists.
Consideration Three: Service Expectations May Include Both Clinical and Nonclinical Activities
Typically, NES physicians serve in a regional and/or site-specific stroke medical directorship role for a certified stroke center (CSC). These physicians provide coverage at one or more CSCs and may also cover primary stroke centers in larger markets. Primary call obligations range from 91 to 252 days, based on the number of NES physicians; sites of service; and other subspecialty rotations covered, as some NES physicians may have additional call obligations (e.g., trauma, backup, cranial, spine).
As such, depending on the supply of physicians in the community, NES physicians may provide coverage well in excess of a traditional 1.00 FTE. In addition, NES providers perform a wide range of procedures associated with the brain, neck, and spine, including but not limited to the following primary procedures:
- Thrombolytic therapy
- Endovascular coiling
- Minimally invasive spine surgery
- Cerebral angiography
- Carotid artery angioplasty/stenting
When defining service expectations, organizations should analyze the types and amounts of NES procedures being performed to ensure that compensation accurately represents provider effort.
ECG’s New Survey: A Final Tool in Your Compensation Toolbox
Even if organizations account for all three of these factors in their compensation plan for NES providers, the lack of publicly available benchmarks makes it difficult to ensure compensation is fair and appropriate. ECG’s team of compensation and valuation experts, dedicated to niche and emerging specialties, have analyzed our proprietary market data and published the most comprehensive compensation and productivity data for NES, with nearly three times the sample size of any other industry survey.
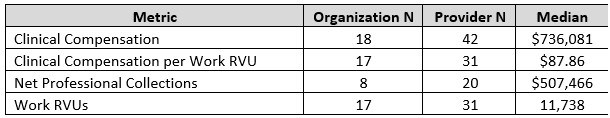
Table 1 summarizes market medians for NES from ECG’s 2023 Physician Compensation and Production Survey.
Table 1: Key Benchmarks: Select Metrics
This compensation and production data will be augmented over the coming weeks with results from ECG’s NES emerging specialty survey, along with additional data and information on this specialty regarding on site clinical coverage expectations, call coverage, leadership roles, compensation model structures, practice profiles, and more.
To indicate your interest in participating in this survey, or for more information on how to gain access to benchmarks for NES and other niche and emerging specialties.
Edited by: Matt Maslin



