If your health system has developed an ambulatory surgery center (ASC) strategy, you’re already heading in the right direction. But executing your plan can be complicated—especially if your organization lacks ASC development and operations expertise.
Before you get to the implementation phase, here are 10 ways to ensure it will succeed.
1. Decide whether to develop a de novo ASC or partner with an existing one.
Many health systems have a blueprint for developing and running medical office buildings and hospitals. But developing a de novo ASC requires specific expertise that systems often lack—not to mention the capital needed to build it and the resources to manage it.
On the other hand, partnering with an existing ASC may present an immediate opportunity to migrate surgery and/or capture value from procedures that are being performed at the ASC and not at the hospital.
- Buying into an existing ASC may offer quick returns, but also comes with limitations—including a less flexible physical plant, challenges securing significant equity, limited distributions, and less operational control.
- Conversely, developing a de novo ASC has a much longer lead time and may cost more, but it allows the hospital or health system to determine its equity position, oversee payer contracting, and design the ASC to meet physician and health system needs with respect to surgery migration, optimization of assets, OR size, and facility capacity.
2. Determine the equity distribution target for the health system joint venture (JV) partnership.
Equity position can have a meaningful impact on the JV structure, governance, management, and overall operations of the ASC.
- If buying into an existing ASC, consider how to structure the acquisition (e.g., stock vs. asset purchase), as this can impact liability and exposure to existing contracts.
- If you’re considering a JV with private physicians or employed physician partners, evaluate the economic implications of case migration on the health system’s existing budget. For example:
- If surgeons migrate cases from the hospital to the ASC, the health system will immediately reduce the cost of care for patients and payers, but also reduce its own revenues. Further, if the hospital establishes a JV with the ASC, it will mean sharing the already lower per case net income.
- If the health system is developing an ASC to generate new volume, a key consideration is where the cases are originating from and what the economic and political impact will be.
- If the health system is seeking new opportunities to coinvest with physicians, private or employed, leadership should consult with legal counsel to ensure the system does not run afoul of any legal and regulatory statutes (e.g., federal or state).
In evaluating the surgical case volume of the entire health system, both inpatient and outpatient, understand the health system’s role in “feeding” the ASC and ensure it is not later paying for value it created. Value creation should be shared across the partnership, and if one partner is going to be more involved in growth, the desired equity percentage should be a significant consideration.
3. Evaluate the impact of payer benefit design and evolution on surgeon site-of-service election.
Review the history of surgical case out-migration to ASCs. Some key questions to answer:
- Are payers denying prior authorizations to surgeons who schedule elective cases in the hospital outpatient department?
- Are health system–employed physicians being denied pre-authorizations due to the lack of an ASC option?
- Are patients being redirected or seeking an ASC as a result of payer site-of-service policies? If so, what is the value of the lost volume?
If the answer is yes to any of the questions above, the health system will likely continue to experience further deterioration of ambulatory surgery volume and redirection of cases. Even though reimbursement reductions are meaningful when migrating surgery volume to an ASC, the long-term value of case retention outweighs the financial impact of losing these cases altogether.
4. Develop a thoughtful and strategic managed care plan.
Health system ASC development programs rely on a solid managed care strategy that allows the health system as well as payers to realize the economic benefit of migrating cases into an ASC. Critical to any ASC managed care plan and payer negotiation is understanding the ASC-eligible volume currently in the hospital/health system along with the financial implications of migrating those cases. Case migration translates to payer savings, but how those savings are allocated depends on the ASC payer contracts. Considering the health system accepts full risk for the capital investment and operations, along with the self-inflicted loss of historical revenues, it seems reasonable for the ASC contracts to appropriately reflect these risks.
Another important component of payer negotiations is the health system’s equity position and management control in the ASC JV. The health system’s equity position will directly impact the ASC JV’s ability to align itself with the health system’s existing outpatient rates. Creating and implementing a managed care strategy in advance of developing these new surgery centers is vital to the overall ASC success, and it is important that this process is led by someone with the appropriate ASC operations and managed care expertise.
5. Identify and engage physician champions.
The success of any ASC will largely be driven by its physician partners, so it’s important to identify the right physician champions. Establishing a JV with physician owners helps ensure commitment and long-term investment in the ASC’s success by actively engaging in operations that optimize efficiency. Optimal physician partners are those who will have a long-term commitment in the ASC, are invested in the community, and are held in high regard as leaders by their peers. Once the right physician partners are identified, involve them in the earliest stages of planning to solidify commitment and attention to the facility’s development.
6. Determine whether the ASC JV will include employed and/or community physicians.
Health systems are experiencing heightened pressure to include employed physicians in ASC JVs. Giving employed surgeons an opportunity to invest in ASCs is a complex consideration when developing the ASC strategy and plan. When developing guidelines for physician partnership, consider the following:
- Are payer site-of-service policies directing patients to surgeons who have access to ASCs in the market?
- Are competing ASCs impacting the health system’s ability to recruit and retain surgeons?
- Is there enough eligible volume to develop an ASC that is solely for the use of employed physicians
- Will your employed physicians support including private community physicians in the partnership?
- How will employed physicians in nonsurgical specialties react to seeing their peers participate in a JV ASC opportunity with the health system?
- What is the health system’s confidence in its ability to backfill cases that migrate to an ASC?
- Are any of the potential physicians who would participate in a partnership already partners at another ASC? What will be your policy about “grandfathering” their ownership in these centers?
7. Build the right team.
Aside from the physician partners, hire the right leadership and operational team. Health systems need experienced, high-performing teams in all aspects of their operations, and entering into a new ASC venture is no different. Successful ASCs consistently deliver efficient, patient-centered care, and are committed to quality outcomes and optimizing the patient and physician experience. Selecting an experienced ASC administrator to lead that team is critical. Depending on the market, finding an administrator with ASC experience may not be easy, so be prepared to invest time and resources in the recruitment process.
Ideally, it is important to hire the administrator at the outset of ASC development. Once hired, the administrator needs to take ownership and be accountable for the successful development and planning of the ASC to ensure it is credentialed and achieves accreditation and licensure as quickly as possible. This accountability will exist organically if the administrator is part of the process. Both the administrative leader and the physician team need to have ASC operations experience and be able to promote a philosophy that reflects the many differences between traditional HOPD and ASC operations.
8. Develop a management plan to optimize ASC operations.
As hospitals and health systems enhance their ambulatory footprint, it is important to develop an effective structure that will foster long-term success. In order to do so, think carefully about your capabilities and any potential weaknesses or gaps.
There are a variety of options for management of an ASC, including partnering with an ASC management company, or developing the management infrastructure at the health system with or without subcontract arrangements with consultants and other advisers. Evaluate how to best provide:
- Managed care contracting.
- Purchasing and materials management.
- Equipment planning and procurement.
- Purchased services that may be subcontracted by an ASC that can be provided by the health system (e.g., biomed, plant management, IT support).
In addition:
- Weigh the pros and cons of an ASC management company, especially if that entity will require equity (resulting in less equity for the other parties).
- If you plan to develop additional ASCs, determine the feasibility of establishing the ASC management and operational infrastructure internally.
- Develop a management services agreement that outlines and delineates the services that will be provided by all applicable providers of management services (e.g., the health system versus a third-party management company and/or consultant).
9. Establish an ASC philosophy and culture.
ASCs have different rules and regulations than hospitals and health systems, which result in different policies and procedures. The philosophy of the ASC should promote a culture that is hyper-focused on efficiency while delivering high-quality care in a cost-effective environment. A successful ASC culture and philosophy centers on optimizing efficiency and collaborating with physician champions and leadership. Hospitals with successful ASCs allow the centers to operate separately, under their own leadership structure rather than treating them like another hospital department. When licensed and Medicare-certified ASCs (not HOPD ASCs) do report to a hospital department, such as perioperative services, they are typically ineffective due to the barriers common to hospital operations that limit the efficiency of the ASC’s operations (e.g., increased levels of meetings, review, and approval processes that impact decision-making timelines).
The most common mistake hospital leaders make is trying to operate their ASC like an HOPD, whether by installing hospital EHR systems, implementing burdensome supply-ordering processes, or requiring multiple layers of approvals and authorizations. As a hospital partner in an ASC, less is usually more when it comes to providing support. It is often best to get out of the way and let the surgeons and ASC leadership manage the center.
10. Allow the surgery center to operate in a manner that is consistent with traditional ASCs and not as a “department” of the hospital.
A hospital can bring many valuable resources to support an ASC, such as managed care contracting, capital, and even some management services (e.g., human resources, plant management, IT support). But an ASC will only have a favorable ROI when it’s able to run as a highly efficient, well-oiled machine. It is important to ensure that the ASCs are not operated under the same cost structure as the hospital.
The traditional ASC organizational structure is flat and allows for ease in operations, which promotes efficiency and can have a material impact on its success. The figure below illustrates the difference between an unsuccessful ASC structure and a successful one.
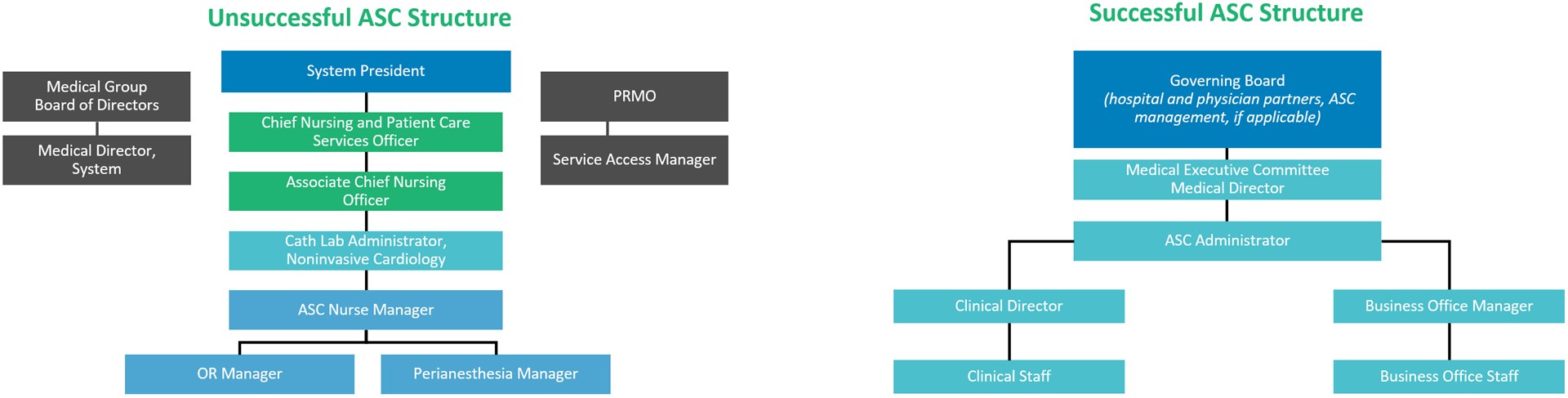
Successful health system ASCs have the autonomy to make operational and financial decisions, maintain strong physician leaders engaged in the operations of the center, and remain focused on both patients and physicians as the customer.
Final Thoughts
Many health systems struggle to develop a separate and distinct ASC infrastructure, rooted in the lack of ASC experience within their organization. Partnering with an adviser with the requisite ASC expertise is critical to avoid mistakes, mitigate potential risks, and accelerate the overall process.



