Effective workflows are the chassis of care delivery, regardless of whether your organization operates under a fee-for-service (FFS) or value-based care model. Well-designed workflows are especially important in value-based care, because these models involve more team members and typically require additional coordination and new tasks.
As organizations begin transitioning to value-based care models, they need to leave their FFS workflows behind. Value-based models need workflows that emphasize communication and collaboration across care team stakeholders to succeed; and prior to implementation, organizations have to reexamine each step in their day-to-day operations and better understand what may need to be be changed or altered.
In an ongoing series, we’re exploring the shift to value-based care and how organizations can succeed under risk-based models. In our first post, we examined the accountable physician enterprise and why it’s a powerful tool to meet success in this growing area.
In this post, we will explore how physician enterprises can operationalize their value-based care plans through redesigned workflows built on value. Redesigned workflows in isolation will not bring the transformation, but workflows that tie together the practice’s goals, staff, and optimized technology will drive high-value care for their patients.
Workflows for FFS vs. Value-Based Care
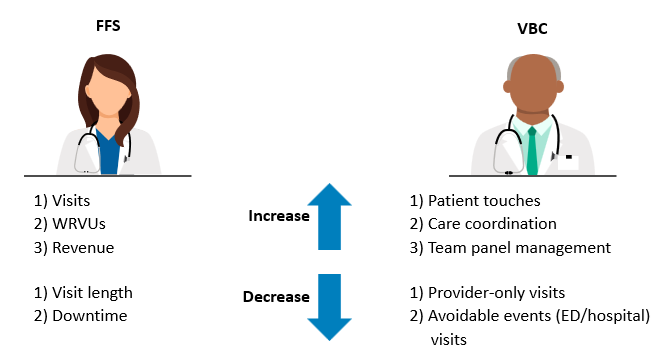
Historically, workflows have been focused on performing high-volume, high-quality patient care and ensuring that documentation reflects the work provided. FFS payment mechanisms produce a transactional encounter, which is reflected in FFS workflows focused on reducing cycle times and maintaining throughput expectations.
Under value-based care, the group’s incentives change—therefore, workflows must evolve to meet new objectives, including:
- Meeting population health goals.
- Integrating team-based care.
- Providing care that reduces avoidable, high-cost events (e.g., hospital admissions/readmissions, ED visits).
Figure 1 shows how the incentives impact the practice under FFS and value-based care as the prevailing forces in each model drive different behavior and outcomes.
While the principles of effective practice management still apply and are, in actuality, more important than ever before, the FFS-based workflow does not position the practice for success under value-based care. Many old habits and tasks have been ingrained in FFS workflows that will now need to be reconsidered. When transitioning to workflows that consider value-based care, organizations must reassign tasks, reduce waste, and streamline processes.
Changes to Ambulatory Operations and Workflows
Taking the above factors and incentives into account, ambulatory groups need to focus on two factors related to their ambulatory operations and workflows when pursuing their value-based strategy:
1. Invest in and develop new capabilities and associated workflows.
- Care management and wraparound care
- Team-based care
- Home-based visits (e.g., home health, virtual support)
- Documentation that supports risk stratification
- Clinical decision support embedded in workflows
- Improved capture of risk adjustment–based elements
- Clinical monitoring and response mechanisms
- Remote patient monitoring in the home and outside of the clinic
- Better access to virtual visits and nurse advice phone lines
- Additional clinical triage
- More effective patient triage, with pre-visit check-in and screening
- Use of virtual symptom checkers
2. Refine existing workflows to align with new incentives
- Redesign in-person encounters to maximize care teams.
- Group visits for education
- In-room triage with clear handoffs
- Improve care team and patient communication.
- Bidirectional communication tools (typically within the EHR)
- Patient outreach and preventive health campaigns
- Increase the use and validity of care protocols and delegation.
- Readdress care protocols and determine whether they still hold for value-based care.
- Determine whether team tasks are still appropriate and at top of license.
- Adjust scheduling rules and policies.
- Acute and same-day visits
- Linked visits with other services, such as dietician and behavorial health specialists
As the practice is reframed to align with the new incentives, the patient journey changes accordingly. Much of the value-added work happens behind the scenes, with the care team conducting pre-visit planning and following up on orders and referrals to ensure the patient receives the services they need. The connection with the patient changes, too, as the practice focuses on maintaining the patient’s health rather than solely delivering care when they are sick or injured.
If a provider organization can develop new capabilities and refine existing workflows to align with new incentives and reshape the practice, it will have accomplished one of the primary steps in becoming an accountable physician enterprise. Effective workflows, coupled with revised staffing models and technology integration, will provide the platform for executing on value-based care operations.
Effective workflows, coupled with revised staffing models and technology integration, will provide the platform for executing on value-based care operations.
Edited by: Matt Maslin


