Many cancer programs continue to face challenges in maintaining access to care given ongoing capacity and resource constraints. This issue will be exacerbated in the future, as projections indicate an additional 11 million patients will be seeking cancer services by 2040 due to the “Silver Tsunami.”
By focusing on core operational imperatives, cancer programs can deliver advanced care and expand access while maintaining a focus on the patient experience. As cancer programs look to the next decade, administrative and clinical leaders will need to implement novel approaches to increase patient access, improve operational efficiency, and ensure equity for all patients.
Across a series of four blog posts, we’re taking a deeper look into each of the pillars foundational to creating a differentiated patient experience, a core element of the cancer program of the future. Part one focused on optimizing patient access, which you can read here. In the second installment, we discuss the importance of incorporating strong patient navigation services across the cancer program.
Problem
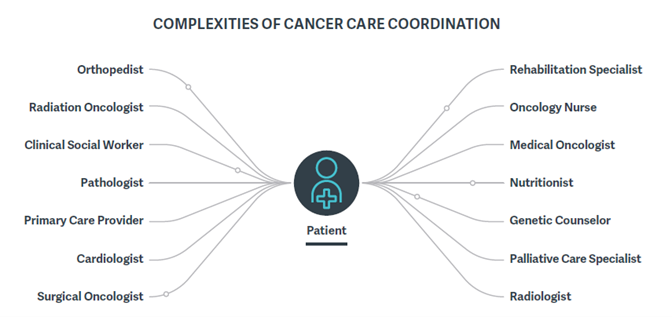
Cancer is a complex disease that requires individualized care pathways, in terms of both providers and events, based on a patient’s clinical diagnosis and treatment plan. This complicates most programs’ efforts to implement a standardized set of care coordination protocols for their entire patient population; therefore, patients often struggle to coordinate care between specialists during their cancer journey. To address this, organizations use patient navigation programs to make the cancer care journey more manageable for patients and their loved ones.
While most cancer programs currently offer some fragmented patient navigation services, high-performing cancer programs facilitate a comprehensive patient navigation experience for all patients, regardless of disease site or geographic location, beginning at the point of intake and continuing throughout the patient’s cancer journey.
There are a variety of areas where enhanced navigation services can buttress existing clinical and operational practices and/or help minimize other patient-specific barriers to care (e.g., language, income, geography, education). These services are particularly important for programs to have in place as a way to efficiently manage patients’ needs as the demand for cancer services increases.
Solution
Given the complexities associated with cancer care, cancer centers should prioritize two key patient navigator roles: the new-patient coordinator and the clinical nurse navigator. These roles are crucial for effectively coordinating care for patients throughout the oncology care continuum.
New-Patient Coordinators
New-patient coordinators are the first point of contact for all oncology patients. They assist throughout the patient journey and are responsible for scheduling appointments and treatments, managing referrals, and assisting with financial matters.
Roles and Responsibilities
- Coordinate appointment logistics for the patient (transportation, parking, lodging, etc.).
- Help the patient complete required documentation, and facilitate the transfer of clinical information to the treatment team.
- Help schedule appointments with support services (financial counseling, social work, etc.).
Clinical Nurse Navigators
Once a patient has decided to pursue their oncologist’s treatment plan, the new-patient coordinator will connect them to the clinical nurse navigator, who will begin to coordinate patient appointments with the patient’s care team.
Roles and Responsibilities
- Accompany the patient to initial appointments when possible.
- Coordinate diagnostics, procedures, and specialist appointments.
- Assess the patient’s physical, emotional, psychosocial, spiritual, and financial needs.
- Provide individual or family counseling and emotional support.
- Connect the patient with community resources, and arrange treatment closer to home when available and appropriate.
In addition to these key roles, successful patient navigation programs will include a strong vision and clearly articulated scope, robust EHR documentation tools, and a high level of physician and organizational commitment. Once established, oncology leaders will also need to determine the most appropriate performance indicators, both clinical and nonclinical, for measuring their program’s success and ROI.
As the demand for high-quality, patient-centric cancer care continues to increase over the next decade, cancer programs must focus on strengthening the four pillars of a differentiated patient experience to continue meeting the needs of their diverse communities, maintain competitive success, and realize programmatic volume growth. In part three, we will explore how provider organizations are integrating innovative digital health tools to support the patient care journey.
For more information, download our whitepaper, Pioneering a Cancer Program for the Future.
Edited by: Emily Johnson



