
October 1, 2014, marks the compliance date for ICD-10. Since the government first announced the move to ICD-10, healthcare organizations have experienced a familiar range of emotions – anger, anxiety, bargaining, denial. Most organizations are finally moving into the acceptance phase. However, despite the compliance date being moved from 2011 to 2014, many organizations either haven’t made much progress on their implementation plans or haven’t started making one yet. Based on a recent study by the MGMA, less than 5% of practices reported making significant headway when rating their overall readiness for ICD-10. This gap poses significant risk, considering that ICD-10 can affect both short- and long-term cash flow and overhead costs if not mitigated appropriately. To that end, preparing for the change to ICD-10 now is essential. The obvious first question is, “Where do we start?”
Establishing the Framework
When addressing any new project, thinking through the various steps – from discovery to planning to testing to implementation – will help your organization identify key areas of concern, as outlined in the figure below.
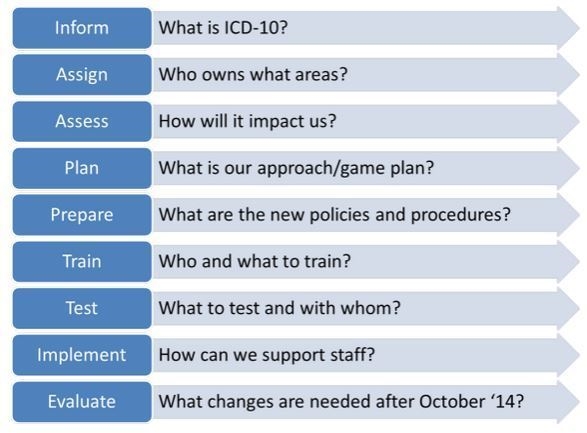
When establishing an ICD-10 implementation plan, it will be important to:
- Evaluate existing IT systems/interfaces, clinical and financial work flows, and reports that currently use ICD-9 codes in order to develop the transition plan to ICD-10
- Develop a strategy for ways to improve diagnosis capture and how the data will be used
- Assess training needs and develop programs to support both the initial and any ongoing training before and after October 1, 2014
- Manage expectations regarding productivity loss, and focus on change management
It will also be important to ensure that a sufficient budget is available for training, resources (e.g., third-party coders to help offset increased coding demands during the first 30 to 90 days of the ICD-10 implementation), and unforeseen financial contingencies.
Tailoring the Plan
Thinking through the life cycle of an ICD-10 code can help define the scope of your project plan and potential areas of impact.
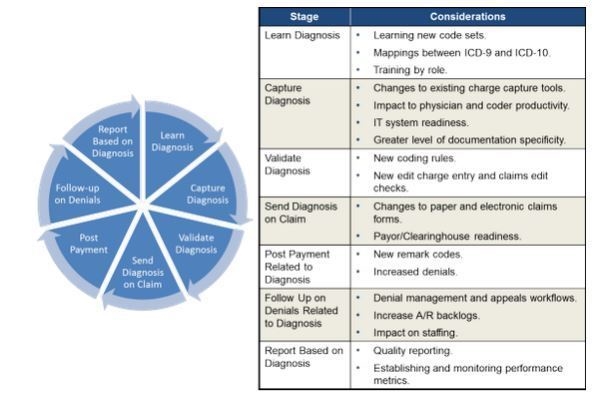
Beyond the standard considerations, such as whether your practice’s IT systems, vendors, clearinghouse, and payers will be able to support ICD-10, it is also critical to recognize the less obvious ways the transition will impact staff. One example is the effect of increased documentation standards on physician productivity, at least at the outset, and the subsequent impact on physician compensation plans that are driven by volume metrics. A second example is the additional communication between coders and physicians to identify the correct diagnosis codes during the first 90 days.
Finally, looking at the experience that other countries have had in implementing ICD-10 can help identify impacts on staffing, finances, IT systems, and partner organizations. The sooner your organization begins evaluating the impact of ICD-10, the sooner you can develop your approach and risk mitigation strategy.
Conclusion
Ultimately, the single greatest step in successfully making the transition to ICD-10 is to act now. Your leadership team must take the time to recognize the challenges the organization will face and devise a strategy to address them. In addition, leadership must champion the cause so that the organization as a whole gains an understanding of the reasons needed to make this change. By connecting with others who are also living through the pain of ICD-10, you can leverage the support of the collective to make it through this experience. Act now so your organization can position itself to ensure a well-planned conversion to ICD-10.

