
Although more than 50% of American physicians now use electronic health records (EHRs), the transition from paper to electronic records has hardly been smooth. A recent AmericanEHR Partners survey found that 39% of doctors would not recommend their EHR system to their colleagues. Moreover, 31% of physicians plan or would like to switch to a new EHR system, according to the market research firm Black Book Rankings.
Healthcare providers often blame their EHR system when the introduction of this technology doesn’t result in both efficiency and quality improvements. But in our experience, the system itself is rarely the primary problem.
More commonly, expectations are not met for other reasons:
- The system installation was seen as a technology project, not an operations project
- Systems were poorly configured and implemented in the first place
- Physician leadership was lacking during the implementation
- No governance structure was put in place to guide decision making and institute best practices
- Process transformation was never properly emphasized
- Effective work flows were never well established
Many physicians believe the solution is to scrap their EHR system and get a new one that is faster and easier to use, presumably resulting in more productivity and less frustration. But that can be wishful thinking, especially in light of the above shortcomings. Before investing time and money in a new EHR system, make sure you’ve maximized the value of your current system. How? By undertaking a comprehensive optimization exercise.
EHR optimization involves continuously identifying and addressing areas of system underutilization, regardless of cause (technical, work flow, leadership/governance, etc.). In addition to enhancing system usage, the initial process can be completed in less than a year, with noticeable improvements in as little as 3 to 6 months. In comparison, an EHR replacement project is likely to take well over a year when the selection and contract negotiation phases are included.
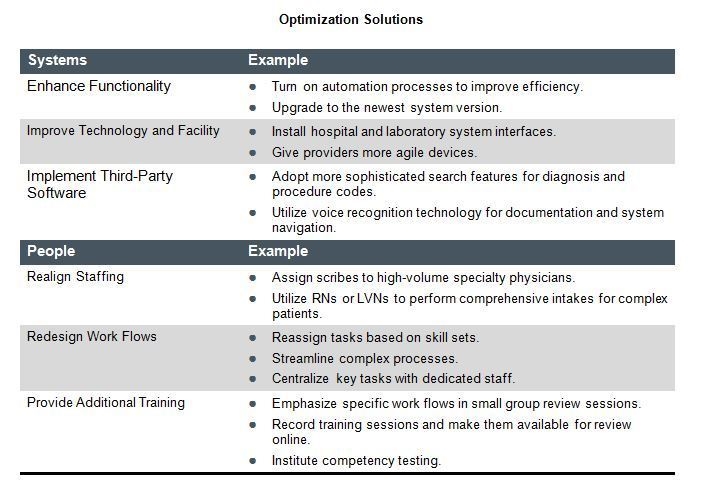
Optimization solutions fall into two categories – those for systems and those for people.
As of early 2013, less than 1% of physician practices had achieved the highest level of system use based on the HIMSS Analytics US Ambulatory EMR Adoption Model; so some level of optimization is possible for virtually every organization. Some solutions will deliver immediate improvement, whereas others involve longer-term structural change. To ensure that your solutions make a real difference, you will need to communicate the plan to all users, prepare them for the changes to come, and keep them fully updated on your progress along the way.
Replacement can be a costly and time-consuming procedure, with no guarantees of improved satisfaction. So slow down, assess your organization’s needs and goals, and try to optimize what you already have. At that point, whether you retain your current system or transition to a new one, you can move forward without looking back.
If you’d like to learn more about why the grass is not always greener with a new EHR system, read the full article.

