
EHR implementation is not for the faint of heart. It’s time-consuming, challenging, and expensive – and not the sort of thing an organization would repeat unless absolutely necessary. As we saw in our post last week, though, replacement is sometimes the most sensible option. Here we’ll describe how to learn from the past and make EHR replacement a success.
Best Practices for Success
Once your organization has decided to pursue EHR replacement, you have a chance to do things differently – and better – based on prior experience. After all, being in the market for your second EHR makes you a more educated and sophisticated buyer. Start by creating a list of required features and functions based on what has worked well and what is lacking in your current system (and don’t be surprised if your next step is shortening or at least prioritizing this list). In our work with organizations purchasing second-generation EHRs, we have observed that they take advantage of the opportunities presented during the selection process, demonstration stage, budgeting cycle, and contracting phase.
- The demonstration stage of the selection effort should be conducted using extensive scripts and scenarios based on what are known to be complex work flows that were either difficult to accommodate with the first system or that continue to be troublesome
- The projected costs should include the unexpected items that arose during the first implementation
- The new vendor contract should represent more than just a document stored on a shelf; for example, if one of the reasons for replacement is poor customer service, pay particular attention to the service-level agreement in the new contract to avoid experiencing these issues again
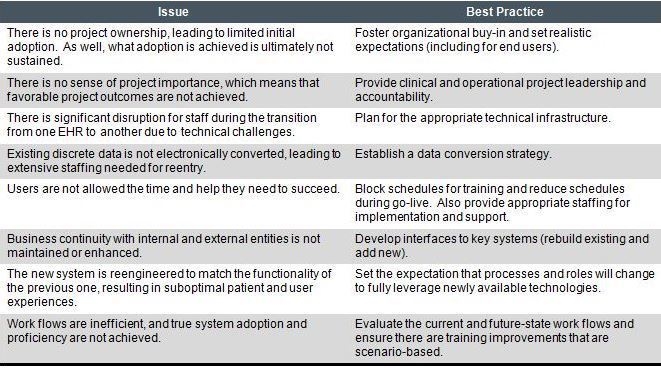
Then, of course, comes the implementation. A successful implementation requires thorough planning and a greater level of technical and training support than is often anticipated. The eight most common issues confronted during the implementation of a replacement system can be addressed by adhering to the following best practices:
Two EHR implementations are one too many, and a third should most certainly be avoided. This means not just selecting the right replacement system and implementing it correctly, but also designing an effective post-implementation methodology for monitoring and optimization over time. System use should be evaluated at predetermined points in the process, such as 30 days after go-live and prior to any significant upgrades. Optimization efforts should be aggressively pursued when there is any indication of declining benefit, such as dissatisfaction, a lack of use, a large list of open support or enhancement requests, or a failure to meet stated objectives.
To learn more about EHR replacement, read the full article.

