
As payment models increasingly shift from volume to value, Academic Medical Centers face additional pressures relative to their non-academic health system peers due to their unique mission of delivering patient care, teaching the next generation of providers, and pursuing medical research. Additionally, AMCs face challenges stemming from complex organizational structures, deeply rooted political and cultural sensitivities, and balancing cost-intensive teaching and research missions.
Despite notable examples of academic institutions that have made early investments in tools and infrastructure that promote clinical integration, early predictions on whether or not AMCs can survive and thrive in a post-reform environment tend to cluster somewhere between “uncertain” and “cautiously optimistic” — even the most bullish prognosticators acknowledge that many will face an uphill battle. Unless AMCs are able to reinvent themselves in this new era, as one chief executive of a leading AMC bluntly put it, “other healthcare systems will simply eat [our] lunch”.
This reinvention needs to begin with bold organizational changes that leverage AMCs tradition of innovation toward the development of organizational and financial structures to achieve greater integration among component entities. The graphic below and corresponding synopsis introduces five specific areas of opportunity where innovative structures can be leveraged to support increased alignment. While these areas are perhaps more conducive to AMCs that are not already fully integrated, many integrated AMCs may be corporately one unit but not functionally integrated. Therefore, opportunity remains for all academic medical centers to examine how they will strike the right strategic alignments to deliver both mission and margins in a value-based care era.
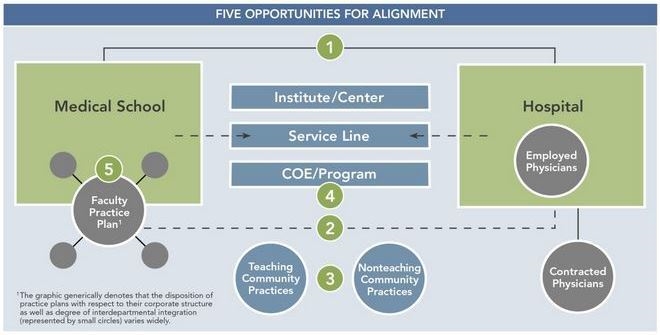
1. Partnership Between University/Medical School and Primary Teaching Hospitals
Many affiliation agreements fail to adequately describe the value of the partnership between the school of medicine and teaching hospital or to clearly define the tangible commitments and expectations that each must provide to promote their mutual success. Opportunities exist to develop more contemporary arrangements, including an overhaul of financial structures to create clear “lanes” of funding for areas such as GME and program development. More innovative shared risk models, whereby discretionary dollars are linked to performance, should also be strongly considered as the days of negotiated “mission support” dollars from the hospital to the medical school, without an understanding of ROI, are over or soon coming to an end. These changes allow hospitals to establish clear value, accountability, and transparency across their investment portfolio.
2. Alignment of Clinical Enterprise Between Faculty Group Practice(s) and Teaching Hospital(s)
AMCs are not immune to the rapid consolidation occurring in the market. The business and organizational relationship between teaching hospitals and practice plans (for those not already under single ownership/governance) arguably represents the greatest potential for tighter alignment for most AMCs – ranging from community-based AMCs to large-scale, well-established institutions. Navigating a growing web of contracts between these entities to balance the economics and growth programs is not sustainable. Instead, these entities should seek to coordinate their investments and share risk more directly to more effectively align financial incentives, and in turn, strategic interests. Additionally, there is a range of contemporary organizational options available that can better align the clinical enterprise while addressing the common concern and false perception that a clinically driven strategy will harm the academic enterprise.
3. Alignment Between Affiliated Community Practices and AMCs
Teaching hospitals with open medical staffs, and those that rely heavily on community practices for key service lines or regional coverage, are as active as their nonacademic peer hospitals with respect to direct employment or exclusive contractual arrangements with community physicians. This raises many questions, and in some cases concerns, for the medical school and practice plan regarding the balance between nonacademic practices and clinical faculty. There are extensive organizational and strategic opportunities to better align the two groups and drive growth of the system, ranging from coordination of outreach strategies to service line development. At a minimum, AMCs should proactively consider how community practices may coexist with academic counterparts and participate in population health management through a clinically integrated physician network.
4. Programmatic Alignment/Integration
The vast majority of high-ranking institutes and Centers of Excellence (COEs) across the country are found at AMCs. However, far too many of them represent only a virtual center or brand, without true strategic and financial alignment. This places AMC-based programs at risk, because without more formal alignment, growth will be stifled, costs will not be contained, and competitors (e.g., community-based programs with a more patient-centered approach), will gain market share. AMCs have an opportunity to design more integrated models for institutes, COEs, and/or major service lines (e.g., heart, cancer, neuroscience, and orthopedics) that creates centralized accountability and aligns incentives between the participating departments and divisions, without undermining the authority of the department chair.
5. Faculty Practice Plan Integration
AMC departments, including clinical departments of many faculty practice plans nationally, are notorious for wanting independence, and it is often difficult for AMC leadership to challenge or change this culture. Understandably, chairs wish to maintain control of nonphysician staff, develop their own compensation policies, retain as much of their bottom line as possible (to the extent its positive), and in many instances independently negotiate contracts with affiliated hospitals. The benefits of having a more integrated and empowered physician organization with practice-wide policies and aligned financial interests will outweigh the short-term, department-dominated view seen at too many institutions today. There are innovative structures that strike a balance between promoting an entrepreneurial spirit in the department and ensuring the broader interests and health of the physician organization. Increased indepartmental integration can create tangible benefits within many practices.
Today’s rapidly evolving healthcare market requires streamlined decision making and organizational structures that support clinical and financial integration. AMCs should be prepared to reexamine their current business models or have their lunch taken.
This post was originally featured on the athenahealth Health Care Leadership Forum – February 10th, 2014.

