
Last summer, CMS released meaningful use (MU) attestation data revealing that 17% of eligible professionals (EPs) who attested for the first-year MU incentive payment of $18,000 did not attest in 2012 to collect the second-year payment of $12,000
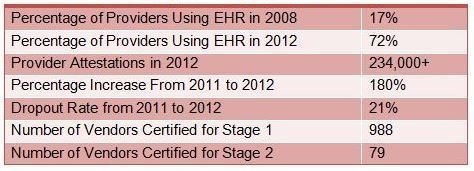
Meaningful Use by the Numbers [1].
When 2013 data becomes available, we will learn whether the meaningful users in 2011 truly dropped out of the program or simply paused their participation to revamp work flows or find more sustainable vendor partnerships. Unfortunately, the financial implications of sitting out for a year are the same as not attesting at all, and penalties will be incurred 2 years after the missed attestation year. For example, providers that successfully attested in 2012 but failed to meet requirements for 2013 will not only lose their 2013 incentive payment – they will be subject to the penalty in 2015 as well.
If the $12,000 incentive in Year 2 wasn’t enough to motivate providers to continue, then we probably haven’t seen the last of this dropout trend – particularly in light of dwindling incentive amounts in future years and more stringent attestation requirements. Additionally, penalties may not be high enough to offset implementation, upgrade, and optimization costs. At a 1% penalty, a provider with $100,000 in Medicare reimbursement will have payments reduced by $1,000 after the first missed attestation year and capped at $5,000 after the fifth missed year.
Cause for Pause
The most apparent reason for the 2011/2012 dropout rate is the change in the reporting period from any consecutive 90 days in Year 1 to a full calendar year of MU data measurement in Year 2. Demonstrating MU of an EHR over a full calendar year is challenging for several reasons:
- Healthcare reform took center stage in 2012 and caused organizations to shift strategic resources away from MU
- EHR software implementations were completed superficially to meet Year 1 requirements with little or no consideration of long-term MU program requirements
- Cumbersome MU work flows that were tolerable for a 90-day period may have become unsustainable for a full-year reporting cycle
- Providers are replacing EHRs in search of more efficient work flows or products that specifically address the needs of their specialty
Stage 2 on the Horizon
Upcoming Stage 2 requirements could result in an even greater decline in program participation. There are concerns that several currently certified vendors will not be ready by the Stage 2 start date. Even those providers who have partnered with a Stage 2-certified EHR vendor will have to work with those vendors to complete version upgrades to Stage 2-certified software. This could further disrupt work flows.
While several organizations (the American Medical Association, the American Academy of Family Physicians, etc.) had come out in favor of delaying the onset of MU Stage 2, it will still begin in 2014 as scheduled. However, CMS and ONC announced in December that Stage 2 and Stage 3 will be extended to allow providers greater time to adjust to the evolving program requirements. Under this extension, EPs wouldn’t need to attest for Stage 3 until calendar year 2017, as long as they have completed at least 2 years of Stage 2.
Stage 2 mandates lab and radiology interfaces as well as HIE and patient engagement technologies, which creates an additional financial burden for organizations already struggling to meet basic MU requirements. While EPs will likely see long-term benefits from following MU guidelines, the short-term costs and work effort associated with the program are likely to cause an increasing MU dropout rate.
For more information on Meaningful Use Stage 2, read the full article.
Footnotes
1. Vendor certification data as of September 2013.

