
Hospitals and physicians are increasingly buying into the buzz around comanagement strategies. But before you dive headfirst into comanagement, it’s important to know how to navigate these relatively uncharted waters. Most comanagement arrangements have only recently been developed, adopted, and implemented. Therefore, healthcare executives and physicians generally lack the experience and insight to fully understand the complexities involved in comanagement development. The lack of a clearly articulated plan and path can quickly derail efforts or lead to difficulties down the road. Based on our experience helping health systems and physicians successfully design and implement comanagement agreements, there are five crucial steps.
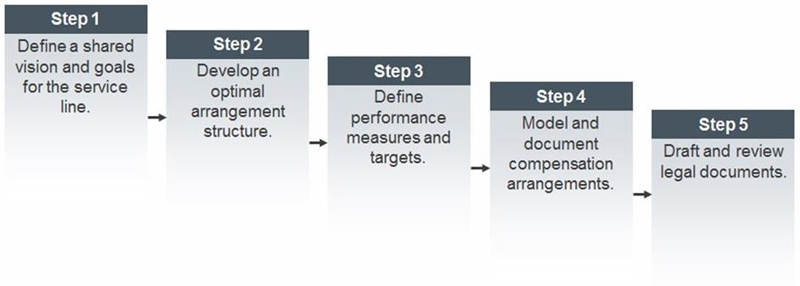
Step 1 – Define a Shared Vision and Goals for the Service Line
It’s important to know where you’re going, and why. A series of interviews should be conducted with key stakeholders to obtain a clear understanding of the priorities, perspectives, and objectives for the arrangement. A steering committee (composed of physician, executive, service line, and operational administrators) can then be created to review stakeholder feedback and articulate a shared vision, principles, and programmatic goals to guide the planning process.
Step 2 – Develop an Optimal Arrangement Structure
A structure needs to be created around the vision. After goals have been clearly articulated and agreed upon, the steering committee should evaluate structural options for the comanagement arrangement. This evaluation needs to address governance structure, subcommittee roles and responsibilities, participant responsibilities, management company formation (if necessary), decision-making processes, and reporting.
Step 3 – Define Performance Measures and Targets
This is the most time-consuming step in the process. The steering committee needs to define specific performance measures and associated metric calculations related to quality, efficiency, patient satisfaction, outreach, and other potential measures. The development of performance metrics will take into account current performance, and parties should aim to utilize measures that specifically address performance deficits.
Step 4 – Model and Document Compensation Arrangements
Then there’s the money. Once the structure and performance metrics of the agreement have been conceptually agreed upon by all parties, the steering committee should develop the financial and compensation arrangements for the participants, including an incentive structure. A third-party valuation firm will eventually be engaged to ensure the proposed compensation arrangement represents fair market value (FMV) for the services provided.
Step 5 – Draft and Review Legal Documents
Enter the lawyers. When the compensation arrangements have been defined and determined to represent FMV, the committee typically works with the hospital/health system legal counsel to draft definitive agreement documents to formalize all aspects of the comanagement program. The physicians frequently engage legal counsel as well in order to review the term sheet/agreement.
The Path Toward a Successful Arrangement
In the current healthcare environment, where some degree of alignment is becoming increasingly necessary, comanagement arrangements can provide considerable benefits for health systems and independent providers alike. However, given their recent introduction to the market, complexity in design, and lack of legislative and regulatory guidance, hospitals and providers must work closely with experts who can walk them through the fundamental steps in designing and implementing comanagement strategies, while also avoiding common pitfalls.
To learn more about comanagement, read the full article.

