
Ever since physicians traveled the countryside making house calls, access to health services has been a cornerstone of effective patient care. Actually providing readily accessible care to the entire population, however, is a goal that has proved difficult to achieve. Expanding access to care and health information is a key priority of healthcare reform, value-based care, and population health management. To improve patient access, health systems and provider organizations must think beyond traditional care models and adopt innovative strategies in redesigning how, when, and where care is delivered.
Rethinking Patient Access
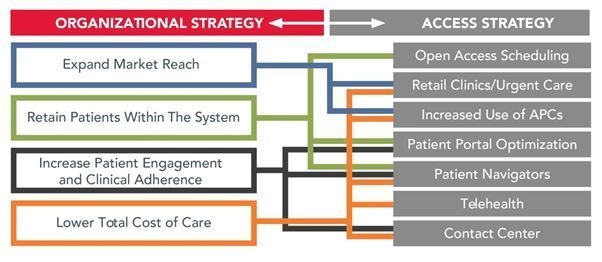
Provider groups are recognizing that the customary model of scheduling routine appointments weeks or months in advance and force-fitting “urgent” appointments into already overbooked schedules doesn’t align with the tenets of accessible care or the expectations of patients. Provider organizations that successfully expand patient access through innovative strategies and across multiple points of entry will be best positioned to reap the operational and financial rewards that come from keeping patients within the system, enhancing patient satisfaction and loyalty, and differentiating themselves from the competition.
So, what strategies are organizations using to overcome operational challenges and improve patient access?
Open-Access Scheduling. Open-access scheduling, which has been around for years, centers on the use of open schedule templates, few restrictions on appointment types, and the elimination of most future scheduling of appointments. Some organizations modify this approach to add more scheduling structure in order to better meet patient and provider expectations.
Expanded Care Settings and New Provider Types. Many organizations have expanded primary care hours in the evenings and on weekends to meet patient preferences and to compete with “convenient care” clinics. Similarly, health systems have begun aligning with urgent care centers and even integrating them into their primary care networks.
Patient Contact Centers. Once reviled as the antithesis of patient-centered care, organizations are turning to comprehensive contact centers to manage the increasingly complex task of getting the patient connected to the right provider. Sophisticated contact centers house a broad range of services, including clinic operations, post-acute coordination, clinical services, and e-Care facilitation.
Patient Portal Optimization. Patient portals have been available for years, but health systems are just beginning to use them to engage patients directly. Common portal features include secure e-mail correspondence between the care team and patient; direct online appointment scheduling; and access to lab/test results, prescription refill requests, and visit summaries.
Patient Navigators. Patient navigator programs are aimed at guiding patients through the complex healthcare system and providing an optimal experience. In their most advanced form, navigators are similar to case managers who help coordinate every step along the care continuum, including both administrative and clinical components.
Telehealth Strategies. Telehealth programs range from technically sophisticated e-ICU monitoring systems to pay-per-use primary care visits via video conferencing technologies, such as Skype. The market is being flooded with non-conventional solutions that provide easy access to medical advice for acute, same-day needs through telephone and Web portals.
Answering the Patient Access Imperative
Patient access problems have long plagued healthcare systems, sending a clear signal that the traditional ways of delivering care simply aren’t meeting the needs of today’s population. Changes to how, where, and when care is delivered are necessary. After all, according to Henry Ford, “if you always do what you’ve always done, you’ll always get what you’ve always got.” And what we’ve “got”, in terms of access, isn’t good enough.

