
The Comprehensive Care for Joint Replacement (CCJR) program proposed by CMS in July 2015 is accelerating the pace of payment reform, and it’s ramping up pressure on hospitals to effectively manage patients and monitor costs for joint replacements.
In a prior In Brief, we provided an overview of the proposed CCJR model. This post spells out the program structure and physician relationship parameters.
Bundle Mechanics
By deciding against a lump sum prospective payment model, CMS is eliminating a potential administrative barrier for most providers. The CCJR follows a retrospective bundle model, in which services related to the joint replacement MS-DRG 469-470 are paid on a fee-for-service basis at the time of service and tabulated at the end of the program year for comparison to a targeted spending amount. The included services will encompass all Medicare Parts A and B care for a 90-day episode (e.g., hospital stay, physician services, drugs, therapy, supplies). The hospital where the patient is admitted is considered the “participant” and ultimately responsible for the shared savings reward or payment owed.
Setting the Target Price
The goal for participant hospitals should be to provide care at or below the target price. The target price and reconciliation payments will be based on a multilayered calculation.
- A blend of hospital-specific historical data and regional data is used to determine the target price, with the regional portion increasing over time.1
- Three years of historical data, adjusted to account for changes in the average performance nationally, will be used to set the hospital and regional target values.
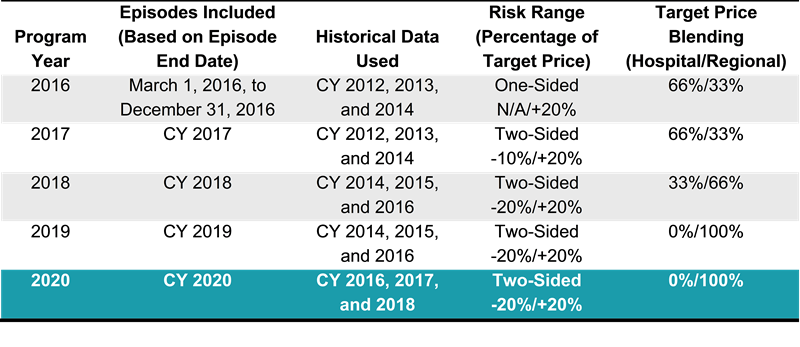
The program will transition the financial risk elements over the first 2 years of the program. Table 1 outlines the structural parameters for the 5-year program.
Table 1 – CCJR Program Structure Summary
As a result of the risk transition and the use of rolling historical data, the target price for a given hospital will change over the course of the program. An example calculation of the target price, excluding the rolling historical data to simplify the example, is included in Table 2.
Table 2 – Target Price Calculation

Understanding the average episode costs and developing mutually beneficial alignment agreements with collaborating providers will be critical to achieving a financial reward.
Collaborator Relationships
The CCJR program provides significant allowances for financial relationships with physicians and other providers (“collaborators”) along the care continuum.2 While hospitals aren’t required to share any savings payments, “gain-sharing” arrangements are expected between hospitals and collaborators. These arrangements may also require collaborators to share in repayments to CMS.
- Agreements must be auditable with a specific calculation methodology, including funds flow percentages and frequency of payment.
- Internal cost savings must be measurable and be the result of care redesign efforts.
Based on CMS guidance, a fair amount of flexibility associated with collaborator arrangements is also expected. Traditional savings opportunities such as supply chain costs and reduced readmission can accrue to the collaborators. Further, collaborators could be rewarded for care process changes that lower the cost of care delivery, such as reducing the number of nurses and surgical assistants present at surgery. The payments made to physician collaborators will be required to follow a structure similar to program-specific gain-sharing arrangements.
CMS is also waiving certain Medicare rules to foster innovation in care process delivery. Relaxing these rules allows for reimbursement of low-cost care to avoid a more expensive emergency department visit or readmission:
- Post-acute home health within the episode period is allowed by waiving the “incident-to” rule so the physician does not have to be present.
- Telehealth visits are allowed by waiving the site-of-service requirements (e.g., the patient would be conducting the telehealth visit from home) and creating a new set of G codes for this purpose.
- The SNF 3-day rule (i.e., minimum of 3-day hospital stay to authorize payment for discharge to SNF) is removed beginning in program year 2, when two-sided risk begins.
The rule waivers invite hospitals to get creative within the care process. For example, a hospital may choose to provide patients with tablet computers to monitor post-surgery progress (e.g., pain, range of motion, vital signs, medication compliance).
The CCJR represents a significant opportunity for hospitals to advance their orthopedic service line and gain financial rewards if they are willing to invest time in preparing their organization and establishing robust partnerships with other local community providers.
Stay tuned for future posts about the strategic implications for hospitals within and around the designated 75 MSAs.
Footnotes
1. See Figure 3 of the proposed rule for the regional designations by state.
2. Collaborators may include skilled nursing facilities (SNFs), home health agencies, long-term care hospitals, inpatient rehabilitation facilities, physician group practice, individual providers (physicians and APCs), or therapists.

