
The patient-centered medical home (PCMH) model has historically focused on primary care medicine. The model was designed to promote comprehensive care – managing acute and chronic conditions, providing preventive services – by improving patient access to a care team. Coordination and integration are the hallmarks of such a team, which may include clinicians (PCP, APC), nurses (RN, LPN), medical assistants, administrative assistants, care managers, social workers, and others. One of the key objectives of such proactive care coordination and management is to keep patients out of more costly care settings, such as hospitals and specialists’ offices.
But the PCMH model does require coordination and collaboration among PCPs and specialists – and that integration is often absent. PCPs are being held financially accountable for the totality of patient care, but are struggling to effectively track referrals and coordinate care with specialists who do not have similar processes or incentives in place. According to the National Committee for Quality Assurance (NCQA), PCPs report sending patient information to specialists 70% of the time, while specialists report receiving the information only 35% of the time. Conversely, specialists report sending information to PCPs 81% of the time, while PCPs report receiving it only 62% of the time. Additionally, 25% to 50% of referring physicians were unaware of when or where their patients saw a specialist.
The reasons for these discrepancies vary, often owing to differences in office hours and procedures, technology, culture, and reimbursement models. But they speak to an overall communication and relationship gap between PCPs and specialists.
This disconnect is irritating not only for physicians but for patients as well. Patients who are part of a PCMH expect the same level of coordination and care when seeing specialists. When this coordination is not present, it too often leads to missed appointments, confusion, trips to the emergency room, and all-around frustration.
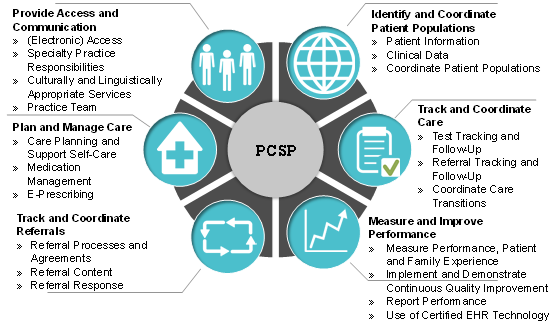
One solution gaining traction is the specialist medical home model. In 2013, the NCQA launched the Patient-Centered Specialty Practice (PCSP) recognition program, aimed at aligning specialty care models with those of their primary care counterparts. The requirements of the PCSP program closely mirror those of the PCMH model and align with other measures and initiatives (see Figure 1), such as the CMS Meaningful Use program and the Agency for Healthcare Research and Quality Consumer Assessment of Health Providers and Systems tool.
Figure 1 – PCSP Requirements
Additionally, an increasing number of reimbursement opportunities are available to further support specialists operating in a medical home model, similar to those opportunities offered to primary care today (e.g., care management fees, bundled payments, global payments).
What this means is that physicians in PCMHs and specialists in PCSPs will be working from the same blueprint in terms of care coordination, care management, and incentives to make care more accessible and efficient. They’ll essentially reside in the same medical neighborhood, thereby facilitating navigation for a patient population that requires both primary and specialty services – and wants the same level of care from all of their doctors.
Though still in the early stages of adoption, there are already more than 700 specialty care clinicians operating in NCQA-recognized PCSPs. And interest in this model is growing, especially among specialties where patients require extensive care across multiple services – such as oncology, hematology, cardiology, endocrinology, and orthopedics.
Next month, we’ll take a look at the medical neighborhood from the perspective of specialists, particularly those who are forming oncology medical homes. And watch for an upcoming article in the AMGA Group Practice Journal in which we thoroughly break down the details and benefits of the PCSP model.

