This month marked the end of the first year of Comprehensive Care for Joint Replacement (CJR), the Centers for Medicare & Medicaid Services’ (CMS’s) first-ever mandated bundled payment program. Approximately 800 acute care hospitals paid under the inpatient prospective payment system (IPPS) are included in the CJR model.
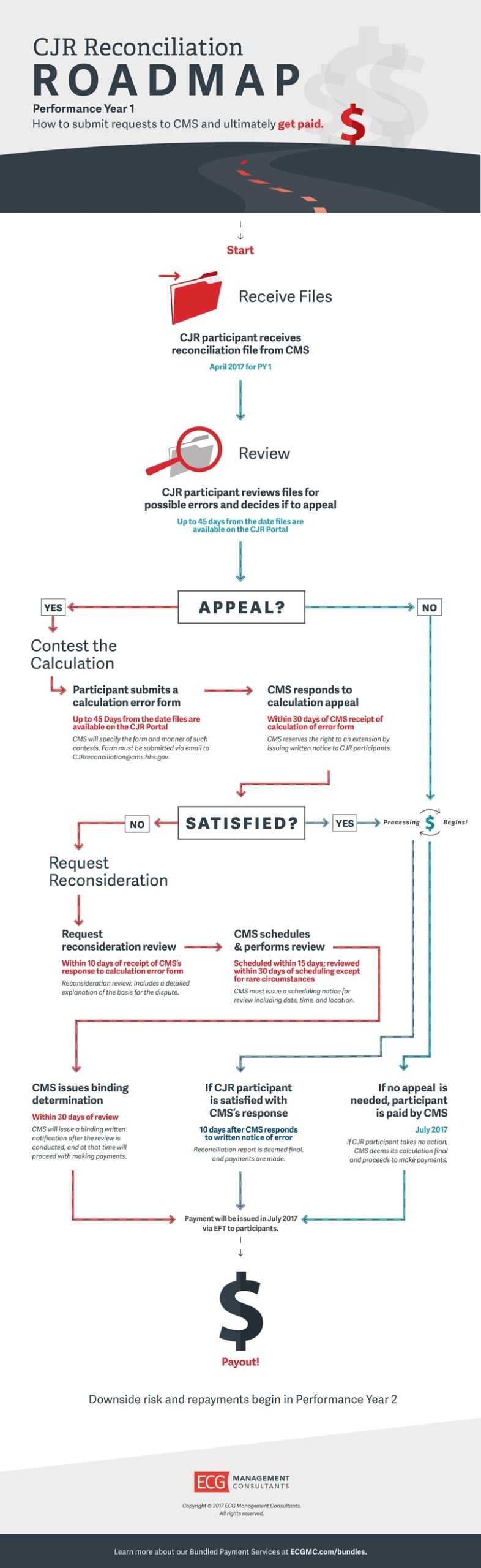
This week, CMS distributed to CJR participants reconciliation reports identifying potential reconciliation payment amounts (where applicable) for performance-year one (PY1) of CJR, which include rewards for quality performance. CJR reconciliation is the process of comparing actual episode spending with quality-adjusted target pricing to determine potential reconciliation payments (or repayment in future performance years) for CJR episodes.
Organizations subject to CJR should be prepared with the following knowledge. Visit our full post over at hfm’s Healthcare Finance Blog.