
On January 9, 2018, CMS announced Bundled Payments for Care Improvement (BPCI) Advanced, a voluntary episode payment model with a 90-day clinical episode duration. This model will test a new iteration of bundled payments for 32 clinical episodes (29 inpatient and 3 outpatient). The aim of BPCI Advanced is to align incentives among participating healthcare providers for reducing expenditures and improving the quality of care for Medicare beneficiaries. The first cohort of participants will start in the model on October 1, 2018, and the model performance period will run through December 31, 2023. Hundreds of organizations submitted applications for the program in March. Applicants are currently waiting for CMS to release claims data and target prices so they can assess their potential performance in the program and make an enrollment decision by August.
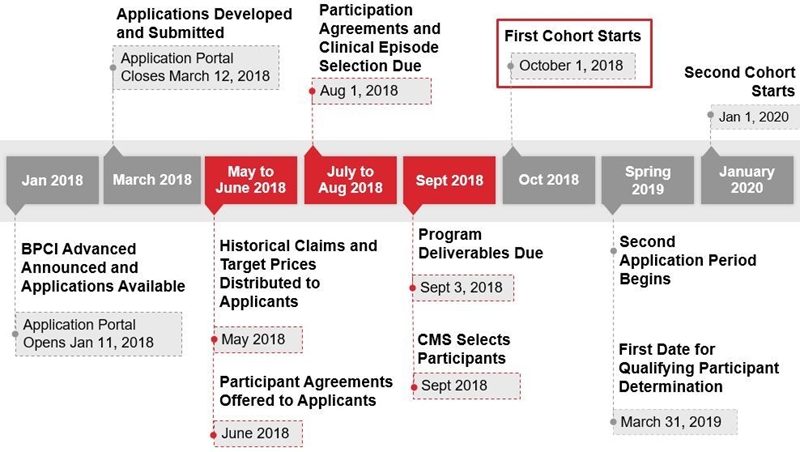
BPCI Advanced Timeline created with information from CMS.
For acute care hospitals and physician group practices that submitted applications, there are three key areas of focus, which are described in the following sections, when preparing for BPCI Advanced:
- Analyze
- Prioritize
- Operationalize
Analyze
The top organizational priority should focus on analysis of the financial and strategic opportunity with BPCI Advanced. In May, CMS will release historical claims data and preliminary target prices for all episodes to applicants. When used correctly, this data can help an organization determine opportunities for success and establish their bundled payment strategy. Organizations can also use the data to project their potential performance in BPCI Advanced. The following parameters should be evaluated in a performance assessment:
- Volume: Does the organization have enough cases in target episodes to warrant selection of the clinical episode?
- Outcomes: How do the organization’s readmissions and/or post-acute utilization rates drive cost in the episode?
- Financial opportunity: How does the organization’s episode cost compare to the target price? Will there be a savings opportunity?
- Care standardization opportunity: Are there service lines that may benefit from additional incentives to either develop care pathways or further refine and operationalize existing pathways?
- Physician alignment opportunity: Are there certain service lines that would benefit from enhanced physician alignment through gainsharing of potential savings associated with bundled payments?
An analysis of these parameters will help organizations understand the true opportunity of the BPCI Advanced program and develop a path for enrollment.
Prioritize
Once a preliminary list of episodes has been selected, hospitals should identify and prioritize opportunities for clinical and financial optimization to ensure effective bundle implementation.
Redesign Care
One of the greatest opportunities to achieve clinical and financial optimization is through care redesign. Bundled payments align incentives among and between healthcare providers by holding organizations accountable to a predetermined target price. This target price can motivate an organization to manage a patient’s care across the continuum. Care redesign is often accomplished through standardization of care delivery, including:
- Engaging physician leaders prior to beginning the care redesign process.
- Documenting and evaluating the current care process for selected episodes (i.e., preadmission, acute care, and post–acute care) and adherence to any preexisting protocols.
- Identifying care process change opportunities (e.g., greatest variation, discharge optimization, internal cost savings, physician practice).
- Creating standardized care pathways based on best practice clinical guidelines (and implementing them within the EHR workflow).
- Developing an implementation plan based on episode prioritization, length of time to implement, complexity, outcomes, etc.
- Identifying key performance/outcome measures to evaluate the effectiveness of clinical and post–acute care redesign across the continuum of care for selected BPCI Advanced episodes.
Care redesign efforts will drive physician engagement, protocol adherence, higher levels of care coordination, a differentiated patient experience, reduced clinical variation, and care that is more cost effective.
Build a Post–Acute Care Network
Since organizations are assuming fiscal responsibility for patients once they leave the hospital, they need trusted post–acute care partners that can help manage patients for 90 days postdischarge. CMS encourages partnership between organizations and post–acute care providers (inpatient rehab, skilled nursing facilities [SNFs], and home health agencies). BPCI Advanced grants hospitals a three-day SNF waiver, which permits beneficiary admission to approved SNFs with an inpatient hospital stay of fewer than three days. This allows providers to discharge patients as appropriate rather than keeping them in the hospital until they qualify for the traditional SNF benefit. This flexibility helps ensure that patients receive proper care in the appropriate setting.
Depending on their market, organizations may choose to enter into formal agreements with post–acute care providers. However, for most organizations, the development of a mutually beneficial relationship is enough to ensure alignment. Organizations can align themselves with high-quality post–acute care providers by selecting those with demonstrated outcomes to comprise a preferred network. By developing a structured approach to managing patients in the post–acute care setting, providers can improve quality and outcomes, ensure the appropriateness of care settings, decrease costs, and increase patient satisfaction.
To better manage patients, hospitals should request and/or collect data on an ongoing basis from preferred post–acute care providers. Organizations can share this list of preferred post–acute care providers with their patients upon discharge and explain why these organizations were chosen (e.g., high-quality outcomes, responsiveness to patient needs, timely communication).
Strengthen Physician Relationships
Organizations wishing to financially reward physicians for delivering high-value care may choose to enter into gainsharing agreements with their providers. While the fraud and abuse waivers have yet to be granted, CMS intends to allow gainsharing under BPCI Advanced. Through these agreements, hospitals can share financial opportunities with providers. Since physician engagement is crucial to the success of bundled payments, gainsharing can both incent and reward a physician’s involvement in care redesign. Physicians decide which post–acute care services a patient uses, so their participation in care redesign activities is crucial—these activities impact the cost of the bundle. Gainsharing provides an opportunity to reward physicians for their efforts. Organizations will have to decide whether these agreements include one-sided risk (i.e., providers reduced spending compared to the target price, resulting in a payment from CMS to the hospital) or two-sided risk (i.e., providers did not reduce spending compared to the target price, resulting in a payment owed to CMS). Hospitals should involve physicians in the gainsharing methodology process to ensure that these decisions are transparent for all parties. This includes deciding whether the agreement will include one- or two-sided risk, which quality metrics providers will be accountable for, and how funds will be distributed.
Organizations will have to identify opportunities with the potential for the greatest success under BPCI Advanced. These opportunities will need to be identified prior to enrollment in BPCI Advanced to improve the likelihood of success and focus organizational resources accordingly.
Operationalize
Proper preparation and monitoring are essential to success under BPCI Advanced. A governance structure and implementation plan should be created prior to the BPCI Advanced start date of October 1, 2018. This ensures that the organization is ready to manage all requirements of the program. Organizations may choose to adapt the structure and plan submitted as part of the BPCI Advanced application and make them more specific to their selected episodes.
Governance Structure
A dedicated bundled payment governance structure provides accountability and helps ensure that all bundled payment tasks are managed and completed in a timely fashion. Ideally, this involves the formation of a bundled payment group cochaired by a physician and an administrator. The physician champion would act as a liaison between the bundled payment group and the physicians to ensure physician engagement. Key responsibilities could include:
- Ensuring executive leadership provides updates and communication throughout the project.
- Overseeing key strategic decisions, timing, communication, and implementation.
- Providing direction and feedback and establishing priorities.
- Allocating resources for implementation.
Implementation Plan
Organizations should develop operational and process improvement recommendations, including tasks and time frames for implementation activities. This plan should include:
- Clear, specific responsibilities to increase effectiveness and avoid duplicate work.
- Smart utilization of existing resources.
- Identification of needed resources.
Analytic Capabilities
Successful participation in a bundled payment program requires organizations to effectively integrate, monitor, and report data. Analytic capabilities may include:
- Working with physician offices on process improvement and standardization that impact all phases of the bundles.
- Coordinating with post–acute care collaborators.
- Identifying and using relevant, actionable data.
- Conducting analytics that support care redesign.
- Deploying risk stratification.
- Ensuring provider adherence to protocols.
- Identifying gaps in care.
- Monitoring and evaluating costs.
- Developing and implementing automated dashboards and reports integrated across all sites of care.
Putting the Plan into Action
Over the next few months, organizations that applied for BPCI Advanced should focus their efforts on analyzing BPCI Advanced data (May 2018), prioritizing clinical and financial optimization activities prior to enrollment (August 1, 2018), and operationalizing their BPCI Advanced program prior to the model start date (October 1, 2018). BPCI Advanced was designed to support healthcare providers that invest in practice innovation and care redesign to improve quality and reduce expenditures. Those organizations that approach the program thoughtfully will position themselves for success.


