Hospitals and health systems are gearing up for a new rule book that could have major ramifications for their cardiovascular (CV) service line and structural heart program. Two key changes are expected:
- New FDA-approved patient indicators that will broaden eligibility for transcatheter aortic valve replacement (TAVR) to lower-risk patients
- Updated CMS requirements for hospitals to establish and/or maintain their structural heart program
If implemented, these changes will have a profound effect on strategy, operations, financing, and physician planning for CV service lines across the country.
Traditionally, TAVRs have been reserved for high-risk patients who cannot handle the stressors of open-heart surgery. However, two studies presented in mid-March at the American College of Cardiology’s Annual Scientific Session offered new perspectives on the clinical requirements for a TAVR program compared to those for a surgical aortic valve replacement (SAVR) program. While they reconfirmed that TAVR is the higher-performing solution for high-risk patients, the studies also concluded that TAVR is at least as effective as open-heart surgery for both low- and intermediate-risk patients.
For hospitals and health systems, the obvious impact of these studies is the immediate growth in TAVR procedures. Currently, there are approximately 60,000 TAVR-eligible patients across the country; when select low-risk patients are included, the pool could increase by more than 33% to 80,000. These new developments will have implications for hospitals with traditional CV surgical programs and hospitals that are already performing TAVR procedures. We explore these implications in the remainder of this blog.
Hospitals Seeking to Establish New Programs
To establish a TAVR program under the current and proposed CMS guidelines, organizations must meet the requirements outlined in figure 1.
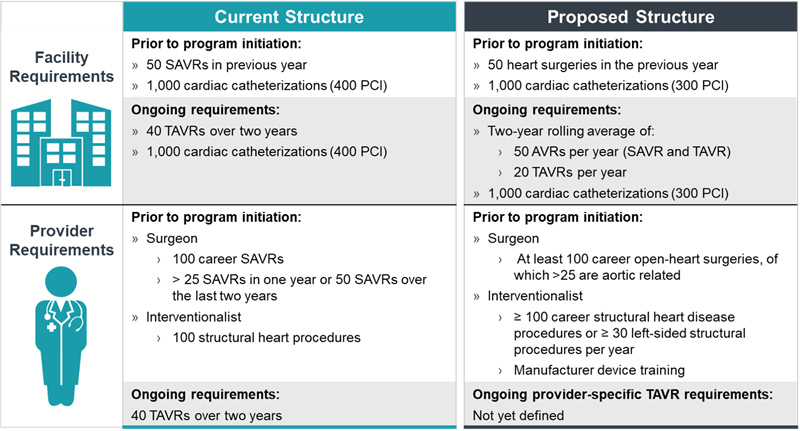
The primary challenge CV service lines have historically faced in developing their structural heart program is the achievement of required CV surgical and cardiac catheterization minimum volumes. The regulations have precluded some hospitals from opening their own structural heart program, a limitation that has been challenging given patients’ increasing tendency to self-select the less-invasive procedure. If eligibility criteria broaden to include low-acuity patients, as recent studies suggest, these organizations will be scrutinizing their CV programs to determine an approach that will allow them to offer structural heart services to members of their community, either independently or in partnership with a regional provider.
Hospitals with Existing TAVR Programs
While programs that offer TAVR reap the benefit of having a structural heart program already in place, broadened eligibility criteria will likely cannibalize existing surgical volumes, as a cohort of patients will now qualify for both procedures. As structural heart procedures gain prevalence, programs will have to judiciously consider workforce planning to maintain sufficient surgical coverage despite likely decreases in surgical volume. And while patients will likely seek TAVR as the less-invasive option, it will be important to develop clear protocols for directing patients to the appropriate procedure type.
Additionally, TAVR cases are frequently seen as loss leaders for organizations that maintain competitive CV programs. While surgical revenues have typically offset those losses, the increased ratio of TAVR to surgical cases may drive down CV service line profitability, at least in the short term as TAVR volumes grow. Consequently, financial management and cost-reduction initiatives should be high priorities for existing TAVR programs to help identify some economies of scale and abate financial shortcomings.
What Comes Next?
TAVR expansion has not been finalized but is the logical next step following the conclusions of the two recent studies. As patients push for less-invasive options, they will self-select facilities that provide TAVR procedures. Offering this capability, when feasible, will be critical to establishing and maintaining a true structural heart program. Consequently, CMS’s new recommendations and the potentially expanding patient pool should be factored into organizations’ CV strategic planning efforts to cultivate leading and financially stable structural heart programs.

