
Introduced in 2013, Total Performance Score (TPS) was introduced as the pioneering fee-for-value (FFV) mechanism with a direct impact on hospital revenue. It conjoins quality and reimbursement by applying earned adjustments to qualifying Medicare inpatient claims through the inpatient prospective payment system. DRG payments are initially reduced by 2% and adjusted upward following application of a complex quality-oriented algorithm. TPS is a function of the Hospital Value-Based Purchasing Program, which is run by the US Department of Health & Human Services with the intent of reducing costs and increasing quality. As detailed below, hospitals and health systems need to understand TPS, how TPS is calculated, and how it can be used to optimize strategic decisions and increase total revenue.
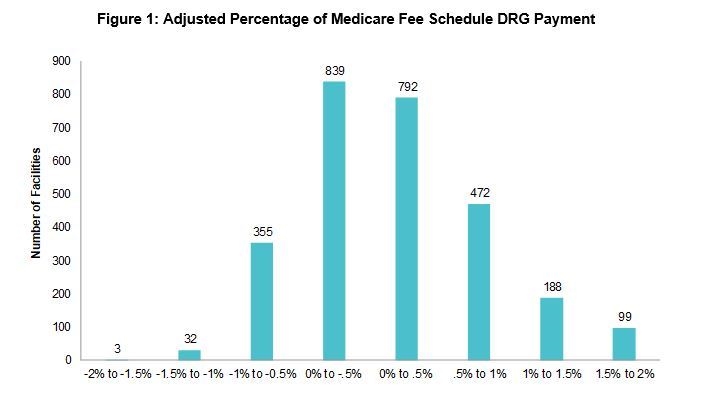
TPS can affect Medicare reimbursement positively or negatively up to 2% for inpatient MS-DRGs. According to the American Hospital Association, 3,000 hospitals nationwide are expected to have their revenue impacted by this program (some facilities without significant volume, including critical access hospitals, are excluded from the program). In 2018, 55% of hospitals received increased payment distributions through the TPS program; in 2019, the total payment distribution is projected to be approximately $1.9 billion. Figure 1 illustrates the adjustment percentages in 2018.
TPS may also indirectly impact Medicaid reimbursement; for example, Arizona requires that 50% of managed care organization payments be tied to value. Further, commercial payers are increasingly tying reimbursement to value. As such, the FFV trend could lead to additional state- and payer-specific programs across the country, many of which will rely on existing iterations, as well as measurement data that has been tested in earlier pilots such as TPS.
Program Structure
TPS points are awarded for surpassing the predetermined benchmark or improving on the previous year’s performance. This incentivizes both continuing improvement and effort, even if current performance is well below the benchmark. However, it also limits upside, as marginal score improvement becomes harder to achieve once high levels of performance have been attained.
To determine value, TPS incorporates four components that evaluate a hospital’s quality, as shown in figure 2. Currently, each category is weighted at 25%.1

Efficiency and Cost
To incentivize systematic cost reduction, the Centers for Medicare & Medicaid Services (CMS) included the MSPB metric in TPS.2
The final efficiency and cost score used for TPS cannot be used to compare costs between hospitals. Groups with lower costs are more likely to attain achievement points; however, over time, improvement points will be harder to gain.
Safety
Patient safety is measured through seven clinical quality metrics:
- Eight select Agency for Healthcare Research and Quality indicators
- Central line–associated bloodstream infection incidence against projection
- Catheter-associated urinary tract infection incidence against projection
- Surgical site infection incidence against projection
- MRSA incidence against projection
- Clostridium difficile infection incidence against projection
- Perinatal care performance as measured by percentage of preterm births (one to two weeks early) when a scheduled delivery was not medically necessary
Each of these metrics is compared to a baseline and to the hospital’s previous performance. Therefore, they cannot be used to directly compare safety between hospitals without analyzing the background data and dashboard. Similar to efficiency and cost points, safety points are awarded for achievement above the benchmark and improvement on the previous year.
Clinical Care
This component focuses on the 30-day mortality (survival) rate for select cases. It is based on the assumption that patients who receive quality care during an inpatient stay will experience improved clinical outcomes and survival rates. The combined survival rate from the following conditions determines the final score:
- Acute myocardial infarction
- Heart failure
- Pneumonia
Factors beyond hospital quality, such as length of stay, post-acute network quality, and care transitions out of the hospital can affect survival rates and, hence, perceptions of in-hospital care quality.
Care Experience
The final TPS component is care experience, as measured by a hospital’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) score. The following eight HCAHPS metrics are considered:
- Communication with nurses
- Communication with doctors
- Responsiveness of hospital staff
- Cleanliness and quietness of hospital environment (two HCAHPS questions combined into one)
- Communication about medicines
- Discharge information
- Care transition (new in 2018)
- Overall hospital rating
Many hospitals already track (and manage to) HCAHPS scores. However, focusing improvement efforts specifically on the above metrics can increase the likelihood of an improved TPS.
TPS provides insight into a hospital’s performance, but it alone cannot be used to accurately compare one hospital to another. TPS can inflate scores for facilities with worse overall outcomes above those of high-quality competitors by reflecting improvement over a one-year period. Conversely, a hospital with excellent outcomes may see its score falter if marginal score improvement requires further investment that is not feasible. Therefore, TPS may be used to highlight a hospital’s year-over-year improvements or its achievement of performance above the benchmark, but using the score to claim superiority over other hospitals would be inappropriate. Find your score here.
Strategic Implications
While TPS has historically been relegated to CMS’s reimbursement methodology, it is increasingly becoming recognized for its strategic implications. In an environment where data can help drive a competitive edge, understanding how TPS is calculated and can be used is vital to organizations looking to streamline costs and maximize revenue.
For example, ECG recently led a 400-bed hospital in the Midwest through a competitor positioning analysis that incorporated TPS findings. Based on the detailed reports, the hospital reviewed a competitive profile of its organization and identified specific opportunities for improvement that would result in a competitive advantage. By understanding the scoring mechanism, the facility was able to prioritize the improvements to maximize impact on the overall score and determine an action plan to maintain a market-leading TPS. The hospital’s analysis, which led to the successful launch of a three-year strategic inpatient improvement plan, focused on three key areas:
- Revenue: Due to TPS’s role in value-based purchasing, changes to a hospital’s TPS directly affect revenue through the reimbursement adjustment applied by CMS.
- Costs: TPS quantifies cost performance and allows hospitals to understand unique strengths and weaknesses, which is particularly relevant in identifying improvement opportunities.
- Improvement Initiatives: Because improvement influences a portion of TPS, TPS can drive decision-making by detailing where strategic investments will deliver the highest return on inpatient revenue.
These efforts were then considered in sequencing resource allocation and incorporated into the hospital’s strategic plan. TPS is a leading aspect of the transition to value and will continue to evolve and influence other FFV programs.
Contact ECG to learn how your organization can fold TPS considerations into overall strategy to maximize the impact of investments and increase total hospital revenue.
Footnotes
1. The weighting and metrics of the components are subject to change year over year.
2. The payments included in MSPB are standardized and adjusted to remove variations due to geography and patient health status.

