
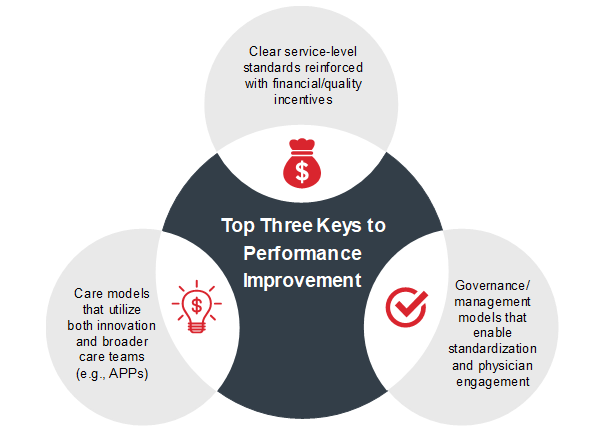
Over the last decade, health systems have faced heightened demand to increase financial support in hospital-based physician services. Whether it be hospitalists, anesthesia, radiology, or other “-ist” specialties, these services now represent a substantial investment for health systems. While many hospital executives view the support as a sunk cost, if services are structured properly, they can act as a major catalyst for driving performance improvement. Figure 1 shows the key factors to drive performance improvement at your organization.
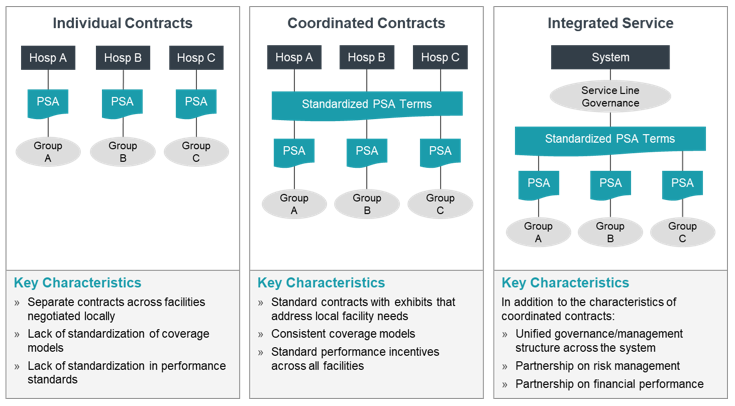
As health systems face pressure to drive better patient outcomes and reduce costs of care, a key focus area to attain results should be the integration of hospital-based services across care settings. Foremost, health systems need to move from disparate contracts/arrangements to an integrated model with standardized contract terms, service line governance, and incentives that supports system-wide initiatives. Figure 2 illustrates a pathway for getting to an integrated hospital-based service, and several case studies provide further detail about how health systems can achieve this integration and performance improvement.
Click on the links below to review case studies on how several organizations have achieved significant performance improvement by advancing their hospital-based physician arrangements.
Case Study One: Anesthesia Services
Regional system in the Midwest that restructured contracts with several independent groups to standardize the coverage model, funding methodology, and incentives across the system
Case Study Two: Radiology Services
Integrated delivery system in the West that standardized contracts and created a system-wide guidance council
Case Study Three: Hospitalist
Regional system on the West Coast that restructured contracts to create unified clinical governance and standard contract terms among several independent groups for hospitalist coverage
An Imperative for Partnerships
When optimally structured, hospital-based physician services lead measurable and sustainable improvements to a health system’s operational and financial performance. By transitioning from unorganized, individual contracts to more coordinated/integrated services, systems can share best practices, enhance resource deployment, and more effectively recruit and retain providers. Restructuring contracts to create arrangements that better align with enterprise performance migrates the transaction-based relationship to a true partnership.
Anesthesia Case Study
Background
A multihospital system in the Midwest was interested in evaluating and redesigning its anesthesia coverage arrangements to align them with current and future organizational priorities. The system contracted with multiple independent anesthesia groups for coverage and employed anesthesia providers at several sites. The independent groups did not employ CRNAs and the majority of anesthesia care provided at the facilities was by anesthesiologists. The system’s goals were to:
- Establish best practice clinical coverage models and evaluate opportunities to incorporate a care team model to provide greater flexibility and standardization of the coverage model across the system.
- Formulate recommendations related to the future subsidy levels and payment structure, including the incorporation of performance-based payments in the contract to better align incentives and share risk associated with the performance of the services.
- Evaluate options to create greater alignment and standardization of clinical care and quality across the system.
Process
The system was struggling to manage the disparate anesthesia relationships and individual contracts across the organization. A critical first step was identifying key priorities for the system and developing a common methodology for evaluating resource requirements and contract parameters across the system. Once the priorities were identified, the system could develop a consistent coverage model based on a care team approach, common funding principles and parameters, a common set of performance metrics to drive greater alignment, and standard service requirements and expectations. The system is successfully migrating to a coordinated contract approach, which will provide the foundation for developing coordinated governance and an integrated service in the future.
Outcomes
The system is in the process of implementing the care team model across the system. Given the change in staffing mix and the need to recruit a significant number of CRNAs, we developed a multiyear transition period with financial incentives for the anesthesia groups to transition to the new model. As part of the transition period, the system is reducing the overall subsidy paid for anesthesia coverage and introducing performance-based metrics, including quality and OR-efficiency metrics, to drive greater alignment with organizational performance and goals.

Radiology Case Study
Background
An integrated delivery system with over 20 hospitals and a large health plan identified imaging services as a key strategy for improving quality and better managing costs across the system. The system conducts over 5,500 imaging exams per day, and roughly 50% of all patients receive an imaging exam. As the organization pushed forward into a value-based environment, aligning with radiologists became a core element to achieving their desired outcomes. Specifically, the system’s imaging goals were to:
- Tightly align all radiologists through performance-based contracts or employment and remove conflicts of interest.
- Establish payment methodologies for employed and contracted radiologist partners that are consistent.
- Develop a unified governance structure.
- Develop physician leaders within the governance structure.
- Create and deploy radiologist performance standards.
- Work with radiologists to develop clinical best practices.
The organization had historically contracted with nine different radiology groups, representing over 100 radiologists, to provide diagnostic and interventional services across the system, and most of the groups desired to remain independent.
Process
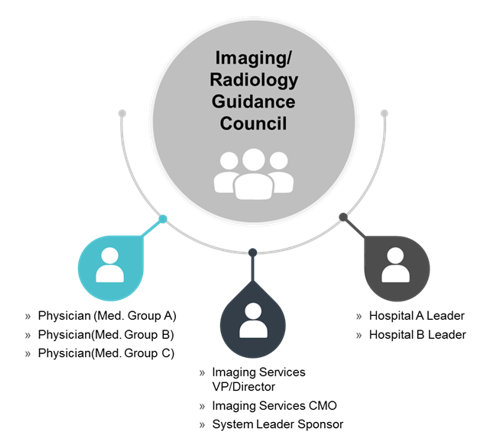
The system’s long-term goals were to enhance the value of imaging services while also creating greater alignment with radiologists. Applying a common set of practices and philosophies to each of the radiology group discussions ensured a consistent framework across all aligned groups. This included a consistent set of alignment options, common compensation principles and parameters, standard service requirements, and representation on a centralized management and governance body. The centralized management and governance structure supports standardization across the integrated service.
Outcomes
The health system successfully employed or implemented a comprehensive professional services agreement with each of the nine groups. The contracts were unique to each group but included the same terms. The health system now bills and collects for all professional radiology services, which allows the organization to bill globally and more easily enter into value-based or risk-based payer contracts. By constructing the financial arrangements this way, the system was able to create a common compensation system across both employed and contracted radiologists, helping to eliminate perceived financial barriers and integrate the groups into a more cohesive service. A system wide committee known as the Imaging Guidance Council was created and now serves as a critical structure for integrating the various groups. The Council also works to manage appropriate utilization, rationalize services across the system, approve system-wide clinical protocols, create level-loading parameters, and establish annual goals (both clinical and administrative). Furthermore, the system is now capable of implementing value-added services such as decision support tools; radiational safety measures; and one-call scheduling, registration, and pre-authorization. In short, the strategy allowed imaging services to become a value generator, not just a volume generator.

Hospitalist Case Study
Background
A regional health system, located on the West Coast, was interested in creating greater alignment between the various hospitalist programs that served the organization’s five acute care hospitals. Although the hospitals were all located in a single metro area, each facility had established its own hospitalist program, which were operated by independent medical groups that held individual coverage agreements. This resulted in a decentralized approach to hospital coverage at each facility with little to no sharing of best practices and resources among the groups. In addition, the health system faced negotiating five distinct professional services agreements every two to three years that each had different terms.
While these programs were successful in covering the adult inpatient needs and working with the respective medical staffs, health system leadership recognized the opportunities to elevate performance if a more coordinated and integrated approach to the system’s hospitalist program was attained. Beyond the operational and clinical advantages of better integrating the various programs, there were additional benefits associated with standardizing the PSA terms. The health system asked ECG to define the optimal organizational structure and financial terms to facilitate the integration of the hospitalist programs.
Process
To establish a coordinated, system-wide hospitalist program, ECG first completed an assessment of the current state, including evaluating the organization and governance structure for each hospitalist group and benchmarking operational and financial performance. Once the gaps in current performance relative to best practices were identified, the system was able to define priorities for the contract renewals. A standardized funding model was then developed that aligned performance among the parties and offered the hospitalists additional financial support for improved performance in key performance metrics. In addition, a performance dashboard was created to report key operational and financial metrics to measure performance across the five sites and facilitate ongoing sharing of best practices.
Outcomes
In collaboration with hospitalist and health system leadership, ECG defined a new operating model that centralized the hospitalist programs into a single division with dedicated management and physician leadership. Under the new structure, the medical groups would retain their individual professional corporations, but functionally integrate the hospital programs under system-wide service line construct. This new division included formal organizational elements that brought the physician leadership across the five sites together to share best practices, define physician recruiting needs, and coordinate coverage. Additionally, the implementation of the standardized funding model resulted in less administrative work tracking and reporting financial performance. The standardized funding terms resulted in parity among the groups that enhanced the system-wide recruiting and retention of hospitalists.



