
If you’re a hospital administrator, you may have experienced the following scenario: a physician returns from a conference, eager to start using the latest implant, robot, or other technology. Good news! They’ve already talked with the vendor and can have the new item by next week. Your mind jumps to the logical question: “How much does it cost?” The physician probably doesn’t know.
Whether it’s a shiny new tool or a reliable standby, physicians tend to have strong preferences when it comes to their medical supplies. But for many physicians, supply costs can be a mystery. Asking them to consider alternatives to high-cost items can be uncomfortable. If these conversations are not approached carefully, physicians may feel they are being expected to cut corners and provide subpar clinical care in the interest of preserving the bottom line.
By approaching the conversation respectfully and with transparent, objective data, you can make your physicians exceptional partners in evaluating the supply costs in their area and helping identify cost-saving alternatives that are clinically appropriate.
Below are 10 ways to ensure those conversations are productive.
Start by increasing awareness. Transparency and education should be the foundation of these conversations. Be sure to give your physicians the benefit of the doubt—they may reach for a $5,000 stent during a procedure instead of a comparable $1,000 stent simply because they’re more familiar with the pricier item.
Make sure you have accurate data when approaching providers. Bad data can do more harm than good and draws your credibility into question. Inaccurate or incomplete data may elicit a defensive response from providers, who often have a clearer picture of the supplies they use than the data may reflect. Before approaching providers, preview and validate data with frontline staff and department administration. Approach conversations with an inquisitive nature: “Based on your experience, does this look right to you? If so, how do you think we could best approach this as a team?”
Try framing costs in a way that resonates with physicians. Don’t talk about the hospital’s bottom line; focus instead on the issue of passing costs along to patients. More expensive items can mean higher costs for patients who may not be able to afford them—this matters to physicians. Enlisting a well-respected physician to initiate the conversation with their colleagues can also help open the door for conversations around change. Peer-to-peer discussions tend to foster open dialogue and decrease resistance to cost discussions, resulting in quicker engagement and the achievement of consensus.
Share with physicians the volume and cost of items they use compared to those of similar items . Focus on frequently used supplies or those with high price tags. Comparing a physician’s supply usage with peers can be eye-opening. If possible, go beyond the walls of your institution and share supply costs for colleagues at other health systems. In some cases, a physician may, indeed, perform more complex procedures on sicker patients and require more complex tools. In other cases, physicians may perform similar procedures on like patients, and the supply cost variation is based on preference. This distinction is not always clear in the data and may require more in-depth discussions to discern. Using the data as a starting point helps begin these conversations productively. Include outcomes data to show that clinical results are not negatively affected by lower-cost alternatives used by colleagues.
Ask for physician feedback. Provide information on lower-cost alternatives, as appropriate, and seek to understand why physicians are using current items. Always ask the physician if there is a clinical reason why an item is preferred. Is it safer? Does it produce better outcomes (e.g., quicker recovery time) for the patient? Does it make the surgeon more efficient? Make sure to understand the investment required in physician education to transition to a new product. Switching items means educating providers and staff, which includes a learning curve, and should therefore not be done frequently or arbitrarily.
Pick your battles. Physicians will likely be amenable to changing some frequently used or high-cost items if clinical results are not compromised, but other items will be viewed as significantly more effective. Don’t challenge every preferred item. An item may be more costly, but if it achieves superior quality and results in fewer patient complications, then pushing your physicians to change their practice is the wrong course.
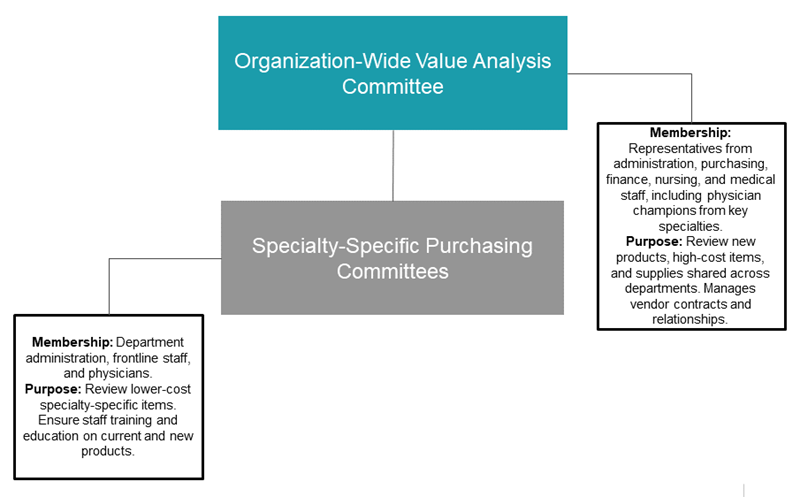
Engage physicians in purchasing committees and supply decisions. This can go a long way toward reducing costs, especially if participating providers use high-cost items themselves. A physician champion should be designated for supply and purchasing activities by service line. In many cases, physicians are interested in learning about supply costs and want to make financially prudent decisions, as long as it doesn’t hurt patients. If your culture supports it, try playing a matching or “Price is Right” type game to lighten the mood.
Seek feedback on the functionality of supplies from clinical staff. Nurses and technicians are often the ones using the supplies, under physician supervision, and will not be shy about sharing their opinions.
Develop a Value Analysis Committee. Create a process for evaluating the use of high-volume/high-expense items and assessing the flow of new and improved technologies and products into the organization. The Value Analysis Committee should include representatives from administration, purchasing, finance, nursing, and the medical staff, and meet monthly to assess the clinical efficacy and financial impact of requested or reviewed items, considering quality, safety, cost savings, innovation, or replacement of existing products.
Consider a test run. Vendors will often provide free product samples to familiarize physicians and staff with new items.
Partnership Pays Off
Reducing unnecessary use of costly medical supplies can decrease overall healthcare costs for organizations as well as patients. By increasing awareness, fostering engagement, and creating an open dialogue, physicians can be your partners in achieving an effective, cost-efficient model that doesn’t compromise clinical care.



