
In a recent conversation with a community hospital CFO, she pointed out that “as surgery goes, so does our system financial performance.” She’s not alone in that sentiment. As hospitals continue to face downward margins, the importance of surgical volume to organizational viability is paramount.
However, surgeons often view hospital-based operating suites as significantly less efficient and user friendly than their freestanding ambulatory counterparts. When physicians choose to perform their cases elsewhere, the effects on perioperative volume and organizational financial health can be stark.
The challenge for system leaders is straightforward: if they want to grow perioperative volumes, they must understand the qualities that attract surgeons to their ambulatory competitors, and replicate them in their hospital ORs. While many health systems begin to address this challenge through traditional lean approaches to identify process inefficiencies in their ORs, efficiency is only part of the equation. Transformative health systems should take a human-centered approach to learn what is most important to their surgeons and design an environment that promotes efficiency and reduces anxiety.
Understanding Surgeons’ Needs
The primary focus of human-centered design is to build processes based on an understanding of what “job” your stakeholders are trying to complete. For surgeons, the jobs to be done are both functional and emotional. The table below outlines just a few of these jobs and explains how success can be defined in a human-centered environment.
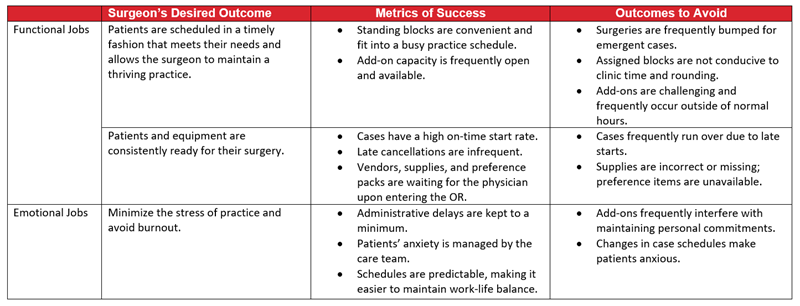
By understanding the functional and emotional jobs that surgeons are looking to complete, it is easy to see why ambulatory surgery options are more appealing than a busy acute care operating suite. The operating hours allow surgeons to maintain a busy practice and have a personal life. The narrower case scope and lower demand for emergent volume make scheduling easy to predict and minimize unplanned disruptions.
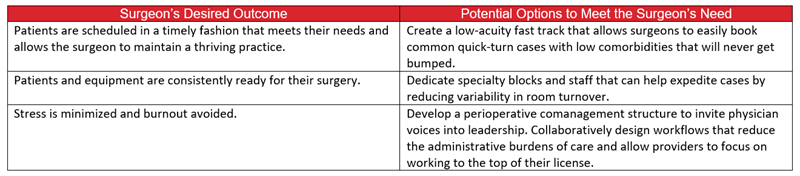
In order to maximize productivity of the hospital-based OR, administrators must be prepared to address the jobs of their busy physicians much like an ASC does. Below are just a few ways to foster an environment where your providers can thrive.
While lean methodologies can deliver significant savings, successful change management relies on enlisting help from all stakeholders to make transformations durable. Starting with a human-centered approach and understanding surgeons’ needs for service and process redesign that meets the goals of all caregivers will allow for change that is meaningful and sustainable.

