
Patient engagement has become a strategic imperative for healthcare organizations across the United States and has been touted as “the blockbuster drug of the century.” The concept of patient engagement is defined by the World Health Organization as “the process of building the capacity of patients, families, carers, as well as health care providers, to facilitate and support the active involvement of patients in their own care, in order to enhance safety, quality, and people-centeredness of health care service delivery.” The lived reality of patient engagement may differ slightly depending on the lens through which it is viewed, but the goals are the same. Patient engagement aims to reduce behaviors that negatively affect the health of patients, like smoking, while simultaneously promoting and reinforcing positive behaviors, such as eating a balanced diet. Motivating patients to actively participate in their own health can be challenging, even when it comes to the most basic things like a yearly checkup. However, the benefits of patient engagement are worth it for health systems and patients alike.
Proven Outcomes
Positive clinical outcomes are a main reason for encouraging patients to become more involved in their care plans. Recent studies have shown that increasing engagement and tailoring care to the patient’s level of engagement contributes to better patient health.
When patients with a chronic disease are actively engaged, mortality rates are significantly reduced compared to control groups. Furthermore, studies involving diabetes patients and patients with heart failure—two high-risk populations—have shown a direct correlation between engagement and adherence to care plans leading to reduced hospitalization incidences and emergency room visits.
To make engagement possible, organizations can offer several tools that enable patients to communicate with providers in a way they prefer. Organizations can do so while contributing to reported scores, such as the Centers for Medicare & Medicaid Services’ (CMS’s) Promoting Interoperability (PI) score through the Quality Payment Program. This score is used by CMS to determine the payment adjustment attributed to each participating organization. Utilizing engagement tools positively contributes to these components, which compose the overall weighted score. For example, providing patients electronic access to their health information makes up almost 40% of the score. Patients benefit from having an online approach to proactively engage in their care plan, while the organization can receive a higher PI score for offering it.
The main draw for organizations, however, should not be the financials involved in these scores—financial rewards may vary each year depending on the number of participants and the score each one receives. Rather, the main draw is that engagement tools, like the patient portal, are avenues to successfully reaching your patients, providing them access to their care and your system. Research conducted by Patient Experience Journal shows that in addition to the logistical benefits of using an online portal, patients experienced psychological benefits tied to increased collaboration and engagement in their care and trust in their providers. In a study focused on patients with diabetes, a positive relationship was established between being registered users and having greater trust and communication with their providers. In essence, by simply providing the tools that patients need, you can increase their level of trust in your care team, which can result in your patients being more receptive to provider recommendations for treatment plans or future visits.
Generational Preferences
Healthcare organizations should keep in mind that a one-size-fits-all approach to patient engagement will not be successful. It is important to understand and address patients’ generational preferences and to recognize that what they want and expect from providers will differ by age. As Christina Hoffman and Jamie DeMaria, PhD, discuss in their whitepaper, although patient engagement shares the same goals across all age groups, how it is understood and achieved varies greatly for different generations.
- Silent Generation or Traditionalists (born 1926–1945)
- Rely heavily on their physician to direct their care
- Tend to have frequent and longer visits due to their level of acuity
- Baby Boomers (born 1946–1964)
- Seek counsel from their physicians, but also do their own research ahead of and after their appointment, as they are interested in reading about third-party evidence
- Often involved with healthcare decision-making for themselves, for their parents in the Silent Generation, and for their children in the Gen Y group
- Gen X (born 1965–1979)
- Generally healthy and assume that their care team will help them make correct decisions for their care
- Most likely to switch healthcare providers based on their most recent experience
- Gen Y or Millennials (born 1980–1994)
- Utilize healthcare services at a low rate; the healthcare services they do access are more likely to be through a PCP, an OB/GYN, or an urgent care center
- Seek health information from multiple places but are less comfortable discussing their health concerns than other generational groups
- Gen Z (born 1995–2010)
- Strive to maintain balance as a part of their overall wellness and are comfortable reaching out to social networks to seek answers about health-related questions
- Guided by the values of their parents, who often fall within the Gen X cohort
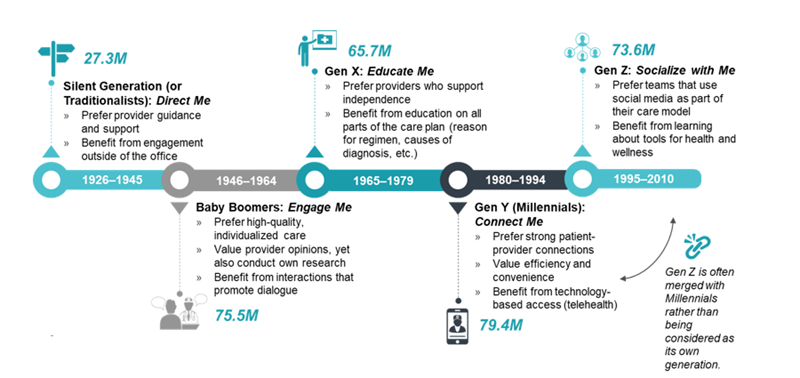
Although there are many differences across generations in the United States, there are some similarities as well. For example, shared decision-making is valued by all people across generations, as is responsibility for one’s own health. Furthermore, people across all generations can utilize technology. Although individuals have varying levels of ability, providers should not assume that older patients are not digitally savvy. Today, 4 in 10 seniors are smartphone owners, which is double the number from 2013.
Motivational Preferences
Motivations can vary based on internal factors driven by a patient’s psychological needs and external factors driven by their environment. Both types can be summarized by Maslow’s Hierarchy of Needs depicted in figure 2 below. This hierarchy outlines the relationship between each factor and the patient’s affected traits. As proposed in Health Standards’ Patient Engagement Is a Strategy, Not a Tool, the application of this hierarchy in healthcare can benefit organizations looking to understand which level most accurately reflects a patient’s current state of motivations.
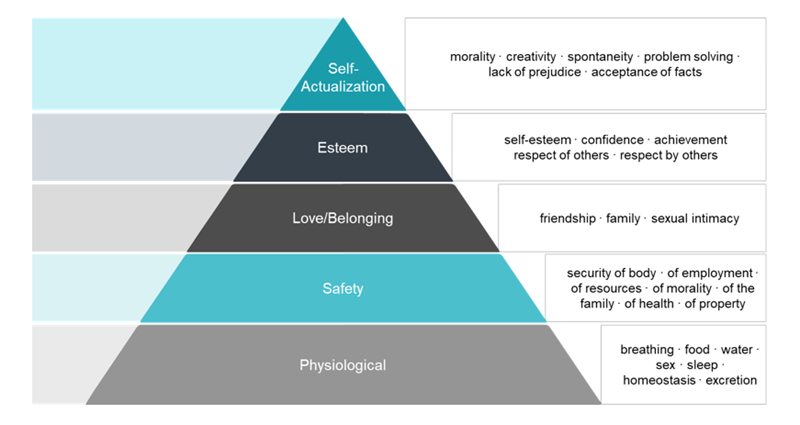
Looking at the factors of each layer, notice how different levels of the pyramid can include both internal and external factors. For example, the Safety layer can be attributed to internal factors, such as security of health, and external ones, such as security of family. The pyramid should be regarded as a spectrum, where patients can fall into multiple levels and be affected by internal and external factors.
Patients on the bottom level are motivated by physical and survival factors. Patients in this level may become engaged due to their desire to fulfill their needs. Next, patients who fall in the middle of the pyramid are least likely to be engaged in their care. This group would most benefit from easy-to-understand details of their care plan to increase engagement. Lastly, patients toward the top are more concerned with factors such as esteem and self-actualization; like patients at the bottom level, they are more likely to be engaged in their care. To them, self-actualization can be realized through patient engagement.
Partner with the Patient Engagement Experts
As emphasis on patient engagement continues to grow, healthcare organizations will benefit by staying up to date on the trends and learning more about their patients. Start by looking at generational and motivational factors to understand the deep-rooted influences that impact a patient’s level of engagement, but also consider factors like culture, geography, gender, sexual orientation, and disability when designing your patient engagement strategy to ensure a holistic approach.
ECG is committed to optimizing the patient experience. Visit our Services page to see how we can help tailor your organization’s patient engagement strategy.

