
Healthcare organizations are under immense pressure to provide seamless care across the entire continuum. COVID-19 has accelerated innovative care models incorporating virtual and alternative sites of care outside of hospitals. The pandemic has also reinforced consumers’ desire to receive care in the safety of their own home, especially among the elderly and individuals with chronic health conditions.
In this environment, home care providers are well positioned to help hospitals and health systems by preventing emergency room visits and rehospitalizations, facilitating efficient and effective transitions of care, and integrating high-acuity services for an increasingly medically complex population in the home.
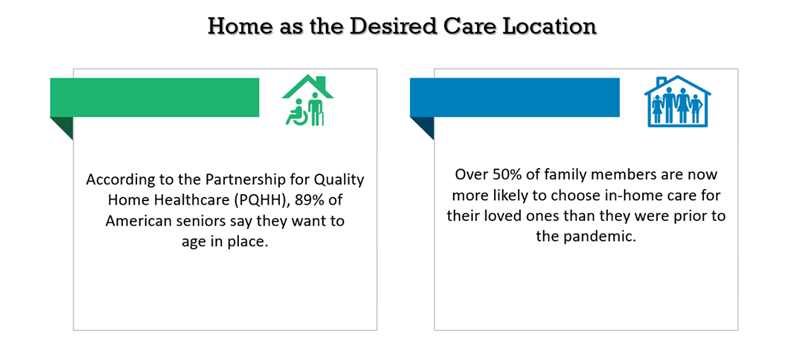
Sources: PQHH, Home Health Care News.
Home health agencies facing financial challenges resulting from the change to the new Patient-Driven Groupings Model (PDGM), along with reduced census due to canceled or postponed elective procedures during COVID-19, need to recoup lost volume and identify new revenue streams for sustainability. At the same time, regulatory and reimbursement changes put in place during the health emergency allow for easier access to home care. While initiated as temporary measures, many of these modifications are anticipated to become permanent as the impacts of the pandemic linger. The growing desire to receive healthcare care at home and the accelerated shift to value-based care, coupled with regulatory and reimbursement changes, represents an environment for innovation and an opportunity for home care services to thrive.
Below are three strategies for growing home care services in the “new normal.”
1. Develop high-acuity, high-intensity services for medically complex patients in the home.
The future of acute care continues to extend beyond the walls of the hospital and expand virtually into homes. Implementing hospital-at-home (HaH) and/or skilled nursing facility (SNF) alternative programs can facilitate growth and expand volume for a home health agency, offsetting COVID-related revenue losses experienced in the first half of 2020 while also potentially lowering the nation’s overall healthcare spend —a win-win situation for all.
Hospital at Home
HaH implementation is gaining traction with the pandemic. Even though traditional Medicare fee-for-service programs do not currently pay for HaH services, many organizations are providing HaH care under value-based and global budget payment strategies for targeted populations (e.g., patients with CHF, pneumonia, cellulitis), where incentives for total cost of care are aligned. By becoming part of the HaH team, home care providers can help meet patients’ needs and position themselves to assist healthcare organizations with the transition to value-based care.
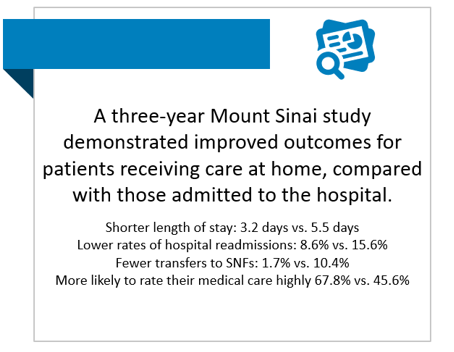
Source: JAMA Network.
Being able to meet the needs of these types of patients means changing the way a home health provider traditionally delivers care. Agencies will need to develop care models that include extended and more frequent nursing visits (twice a day or 1.5- to 2-hour visits); high-acuity services, such as IV therapy and wound debridement; and support services, including nursing aid visits and social work intervention. Integrating into HaH programs also means incorporating telemonitoring and virtual check-ins, as well as coordination with other medical providers such as physicians, PAs, and paraprofessionals.
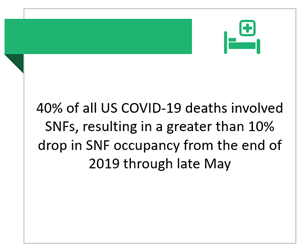
Source: Skilled Nursing News.
SNF Alternative Programs
As SNF occupancy rates continue to decline due to COVID-19, there is increasing opportunity for home health agencies to provide high-intensity care for medically complex patients that would have traditionally gone to a SNF. Successful SNF alternative programs work closely with hospital care managers to facilitate patient data exchange and timely, easy transitions out of the hospital at any time of day or day of the week. Agencies should position themselves to admit patients to home health services on the day of discharge from the hospital, incorporate telemonitoring and virtual check-ins, and develop structured care pathways for high-acuity, high-volume patient populations. In order to take full advantage of this potential increase in volume and not leave dollars on the table, agencies should:
- Ensure the necessary coding skills and resources are in place to capture all comorbidities and acuity of functional deficits for “credit” under PDGM for Medicare patients.
- Optimize processes and increase staff training for accurate and timely clinical documentation.
Incorporating Digital Health
Both HaH and SNF alternative programs require integration of digital health and telemonitoring capabilities. Success with digital health interventions is not just a matter of choosing the right vendor and purchasing the technology. Home health leaders implementing these services will need to develop new, effective operating models for episode management to include coordination of both in-home and virtual visits; resources and structure to monitor biometric and self-reported information from telemonitoring applications; and effective care management and navigation for postsurgical and chronic disease populations. Digital platforms can also be utilized to allow patients and families to proactively request and schedule in-home visits online for a time that is convenient for them rather than deferring to the agency’s schedule, which improves patient satisfaction and reduces canceled visits.
2. Expand the continuum of care to include outpatient therapy.
Home health agencies can provide and bill for Part B outpatient therapy services under a therapy plan of care . If a homebound patient has improved to the point that they no longer meet the requirements for home health services, the agency can discharge the patient and readmit them under outpatient therapy. This will require development of a separate set of outpatient policies and procedures, billing processes, documentation, training, and ongoing auditing for compliance. However, the benefits may well outweigh the effort.
Non-homebound patients, patients who are medically stable but need therapy refinement, and patients who need more visits to achieve their goals are appropriate for outpatient therapy in the home. Delivering outpatient therapy not only provides continuity of care after home healthcare is completed, but also keeps patients within the agency’s network, thereby increasing revenue and profitability. It also provides the opportunity for extended monitoring to reduce hospitalizations with less regulatory, supervision, and documentation requirements than traditional home health services.
3. Diversify into nonmedical home care services.
Incorporating nonmedical support services to address social determinants of health and custodial care needs is another route for generating alternative revenue. In addition to the private pay revenue stream, approximately 245 Medicare Advantage (MA) plans now offer nonmedical benefit coverage for services such as meals, social needs, structural home modification, custodial care, and transportation under the Special Supplemental Benefits for the Chronically Ill (SSBCI). There is an opportunity to branch out to provide such services and negotiate contract(s) with geographically local MA plans. Start having the conversations and utilize data for measures such as readmission rates, fall rates, and patient satisfaction to demonstrate the value of the home care agency for keeping people safe at home and reducing cost-of-care expense for the plan.
Maximize the Current Opportunities
The pandemic and recent regulatory and reimbursement changes have created solid opportunities for home healthcare service providers to showcase their value and innovate to meet healthcare needs and consumer demand. It has never been more important to keep people out of the hospital, and the pace of change has never been faster.

