
Health systems and medical groups have multiple performance improvement (PI) methods available for use, but many struggle to identify how and where to apply these methods most effectively. These organizations often implement a range of PI methods to gain operational efficiencies by focusing on eliminating waste and standardizing processes, but with varying degrees of success.
This is in part because no standard approach currently exists to direct healthcare leaders exactly how and where to align their PI efforts and resources with the pressing needs of the organization. In addition, difficulties often arise when trying to determine the most appropriate technique or intervention to deploy given limited resources.
This post explores how leaders can efficiently identify opportunities to apply PI methods, such as Lean, Six Sigma, and Change Management, so that their application targets high-priority processes that are relevant to delivery of a high-quality patient experience.
Identifying Performance Improvement Opportunities
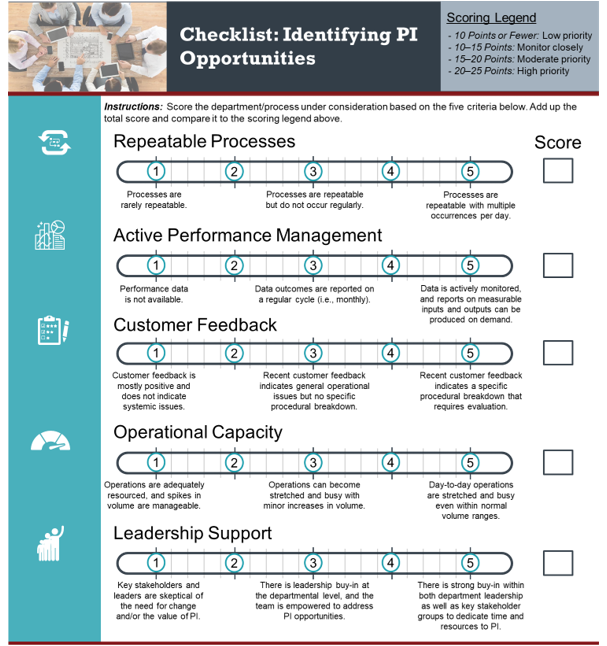
While many PI methods are rooted in a management and operations philosophy that may unlock value and support a culture of continuous, organization-wide improvement, it is important to understand which operational areas are best suited for PI techniques and culturally prepared for change. Departments or processes that should be prioritized for PI support include elements such as the following:
Repeatable Processes with Multiple Occurrences per Day: Many departments execute the same daily processes originating from a limited set of inputs. Repeated processes lend themselves well to being mapped and analyzed to determine where pain points, waste, and variability exist within a workflow. Mapping a process is the first step in determining what the standard is, should be, and could be with a PI effort.
- Example: Hospital laboratories repeatedly perform the same portfolio of tests on a daily and weekly basis; however, prolonged turnaround times resulting from bottlenecks or waste in the process leave providers, and subsequently patients, frustrated and waiting.
Measurable Inputs and Outputs: The availability of measurable data is critical for evaluating whether any PI effort is leading to improved operations. It is equally important to review leading measures, in addition to key outcome indicators, in order to evaluate overall process health.
- Example: Central sterile processing departments benefit from a PI perspective for having a highly measurable process from, receipt of a pick list to sending the case cart to the end user.
Customer Feedback Indicating a Need for Evaluation: Receiving consistent negative feedback from patient or provider customers regarding turnaround timeis an indication of the need to evaluate workflow inefficiencies and improve customer service. Feedback regarding undesirable outcomes not related to turnaround time, while sometimes subjective, may also indicate a breakdown in the value-delivering processes.
- Example: Hospital supply chain operations suffering from inefficiencies in logistics, order processing, and order receiving can frustrate internal customers and delay critical supplies and equipment reaching the patient care areas.
Day-to-Day Operations Often Feeling “Stretched”: Departments feeling overwhelmed or stretched despite a normal range of volume inputs are likely suffering from a workflow issue such as a bottleneck within the process. This misalignment indicates a need to evaluate the process.
- Example: Pharmacies use an almost identical workflow for a significant majority of prescriptions and orders, but staff can often feel overwhelmed trying to process and dispense a batch of routine orders.
Strong Leadership Buy-In and Openness to Change: Willingness to change long-standing processes can be difficult but is necessary to be successful in any PI-led engagement. Change management accompanies almost every operational change and is made easier by continuous and visible support from key leaders.
Building Sustained Value Through Continuous Performance Improvement
Guiding operational leaders and teaching them how to apply significant, lasting change resulting from PI initiatives is critical to incrementally building a culture of continuous PI within these ancillary support areas. Improvements can often help systems realize immediate gains but lead to diminishing returns if the appropriate structure is not in place to sustain, and even improve upon, efforts over time. Ongoing measurement and accountability are paramount to the sustainability of any improvement. Outcome, process, and balance measures must be defined and established both before and after intervention to understand the immediate and ongoing impact. PI efforts require leadership and staff to become students of their process; their understanding and focus on the process is important to sustain and continue the improvement. By teaching operational leaders the tools and techniques to be successful in PI, organizations are able to position themselves for long-term, sustainable impacts.
Several examples of PI tools and techniques are as follows:
- Sort, Straighten, Shine, Standardize, and Sustain (5S): While simple in theory, 5S can be a significant first approach for driving out waste and increasing efficiency within a process. This is achieved by creating visually organized work spaces so that a tool or piece of equipment has a place and is consistently returned to its designated space. By doing this, team members do not waste time looking for tools needed to do their job.
- Daily Management System: Daily huddles, Kaizen events, or visual management boards help instill a culture of continuous PI through consistent, visual reinforcement.
- Value Stream Mapping: Creating a workflow detailing all user steps in a process yields critical insights into waste and opportunities for improvement.
- Standard Work and Visual Management: Standardizing key processes step by step, coupled with visual cues and job aids, helps eliminate variability within a process and promotes best practices within a department.
- Rapid Cycle Improvement (Plan-Do-Check-Act [PDCA]): Also known as the Deming cycle, this method details a four-step Lean framework for incremental change, adjustment, and implementation.
While this is not an exhaustive list, these techniques provide the groundwork to help ensure that continuous PI becomes ingrained in the fabric of the department as opposed to a singular project or set of projects.
Building a Foundation for Sustainable Results
Any health system or medical group’s strategy for PI must include a clear process to evaluate and prioritize departments and workflows based on their suitability for PI resources and readiness for change. Educating operational leaders to deploy PI tools and techniques, regardless of the chosen philosophy, will pay short-term dividends while building the framework for a sustained culture of continuous improvement.
ECG supports performance transformation to maximize opportunity and minimize risk.
Contact our experts.
