While the importance of patient access is generally recognized, healthcare leaders face a problem that may be surprising: no single, nationally accepted metric or benchmark exists to measure it. When discussing access, the conversations surrounding which metric to pursue are largely dependent on what data has been historically available to a health system. Even more, systems may disagree about what access should measure, balancing when patients want to be seen with what is achievable by the organization and what is medically reasonable.
Patient access is a health system’s ability to connect the patient to their care team. This is most often thought of as securing a new patient appointment, but it also includes scheduling follow-up care, managing referrals and transitions of care, facilitating communication between the patient and the care team, and other navigation of a patient’s journey.
Measuring New Patient Access
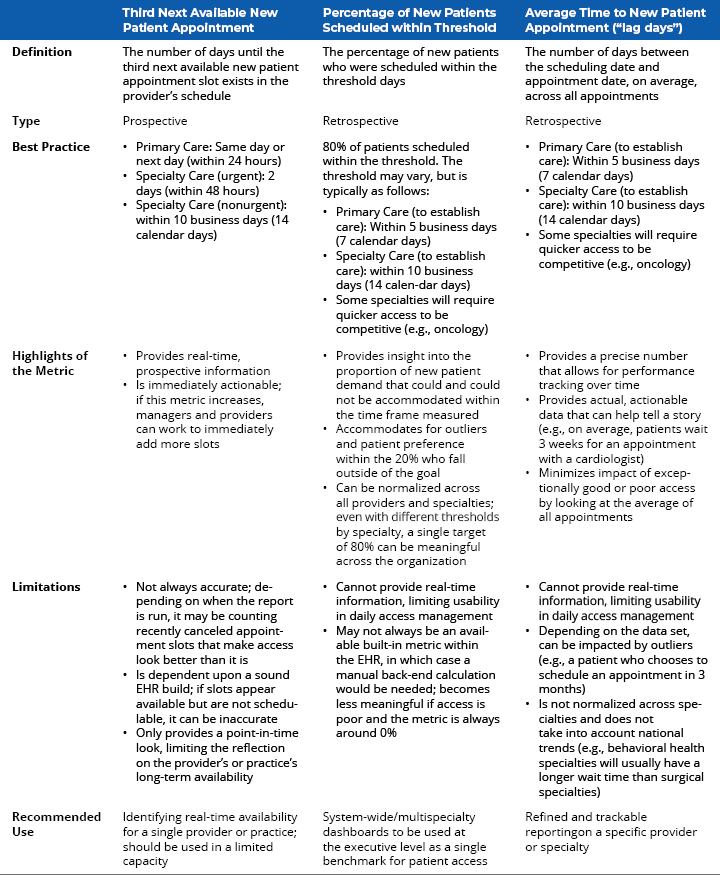
When we focus on the most prominent patient access component, three metrics are most commonly by health systems:
- Third next available new patient appointment
- Percentage of new patients scheduled within threshold
- Average time to new patient appointment (“lag days”)
Measuring access to care in the ambulatory enterprise is essential to the successful delivery of cost-effective and patient-centered care, and metrics provide insight for healthcare organizations to optimize performance. Operational leaders should be looking at all available access metrics regularly.
When health system executives are seeking to choose a single metric to gauge the system’s access performance, percentage of new patients scheduled within threshold should be chosen. This metric provides a cross-specialty view that accounts for each specialty’s need and ability to schedule new patients in a timely manner. This metric should be the metric of choice for executive dashboards.
When monitoring access at a practice or department level, average time to new patient appointment can be a helpful metric. It provides more precise and actionable data that can be tracked over time. Ambulatory leaders will understand the impact of this metric and how it compares across specialties.
Using third next available new patient appointment can be helpful when looking at real-time schedules, as it provides a window into actual availability that patients experience and allows providers and practice managers to take immediate action to add access when needed.
Measuring Other Components of Patient Access
In addition to monitoring time to new patient appointments, organizations should also track metrics that evaluate the patient’s journey through the system, including:
- Referral capture and turnaround rates.
- Provider capacity, schedule utilization, and other scheduling metrics.
- Patient and provider no-show and cancellation rates.
- After-hours availability (i.e., evenings, weekends) of practices and urgent care centers.
- Digital scheduling enablement and utilization.
Alongside the effort to maintain a patient access dashboard, organizations should:
- Monitor patient access consistently (department leaders should review access across visit types weekly).
- Obtain buy-in from their employees and providers to improve access.
- Measure appointment supply and demand across specialty departments and find a balance between the two.
- Ensure there is an adequate staffing and provider workforce.
- Ensure processes and technology are optimized to support intended outcomes.
- Continue to monitor patient access measures, and continuously improve on the key success factors listed above.
In some cases, improving patient access is a multifaceted approach that can require organizational transformation. However, failing to make improvements and investments can result in inability to meet consumer demands and loss of market share in a competitive landscape.
Driven by technology and increased purchasing power, patients are seeking care that is convenient and cost-effective. Learn how patient access at your health system compares to others in your geographic area and why now is the time for ambulatory care transformation.


