With data from the Society of Thoracic Surgery (STS) showing that the total number of adult cardiac surgeries remained relatively flat between 2010 and 2019, it may be fair to question what the future of cardiac surgery programs will look like, and where surgical growth may come from. Consider:
- Over the past decade, advances in minimally invasive procedures and imaging technology have increased treatment options available to cardiac patients, with open-heart surgery giving way to less-invasive approaches.
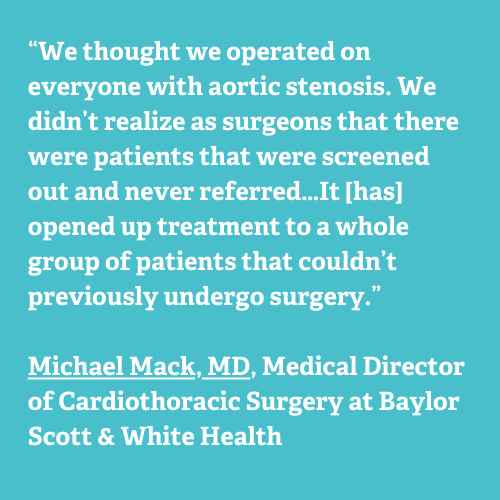
- In 2011, transcatheter aortic valve replacement (TAVR) was first approved by the FDA as an alternative to surgery. Eight years later, TAVR exceeded all forms of surgical aortic valve replacement, a trend that’s expected to continue.
These advancements, along with consumer preference for less-invasive therapies, seem to signal an inevitable decline in demand for traditional open-heart surgery.
At the same time, need for overall cardiac care continues to increase significantly. Population data from the 2020 US census projects that more than 130 million adults—or about 45% of the US population—are expected to have some form of cardiovascular (CV) disease by 2035. This rising prevalence, combined with efforts to provide earlier preventive screenings, will likely accelerate the demand for cardiac care, including surgery.
Below, we’ll explore the implications of cardiac surgery’s changing landscape on surgical volumes, case complexity, and the future of physician training programs—and how CV program leaders can best position their surgical program for growth.
A Shift in Valvular Heart Disease
Adult cardiac surgical volumes may have flattened between 2010 and 2019, but there were significant fluctuations in specific types of surgery during this same time period—most notably with the treatment of valvular heart disease (figure 1).
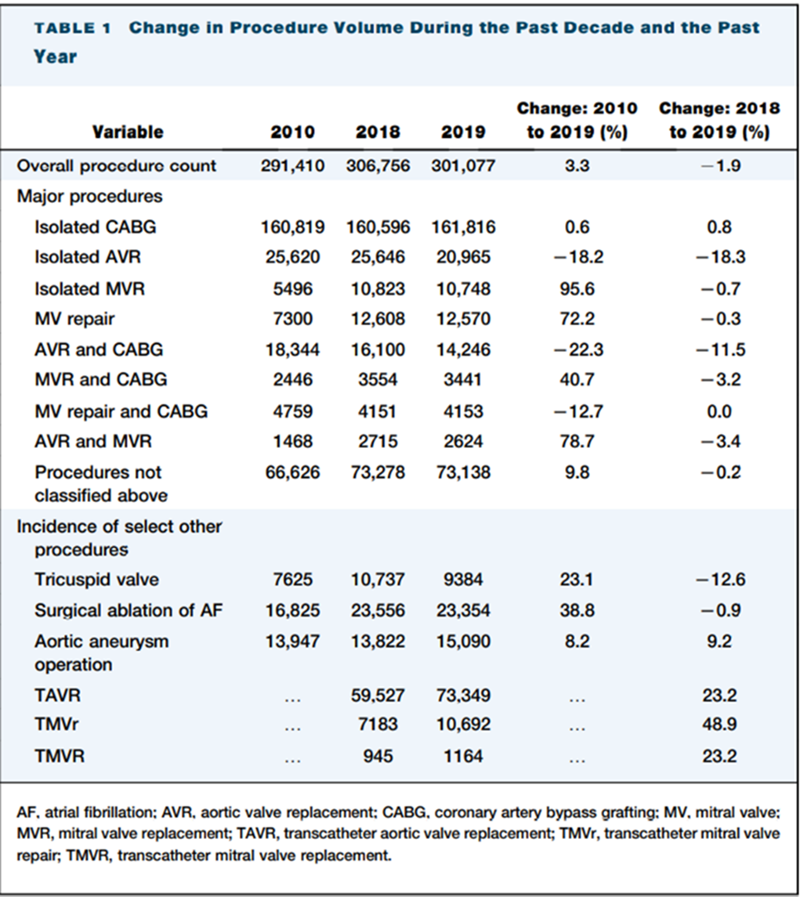
The emergence of TAVR led to a dramatic decline in surgical aortic valve replacements (SAVR), and at the same time, mitral and tricuspid valve surgeries increased 55% and 23%, respectively.
The significant increase in mitral and tricuspid valve procedures can likely be attributed to earlier prevention screenings, as well as the emergence of the multidisciplinary “heart team” construct. The heart team emerged a decade ago as a patient-centric model in which cardiologists and cardiac surgeons jointly evaluate a patient and, through shared decision-making, determine the most appropriate therapy—typically either surgery or a catheter-based procedure. Many CV programs have since adopted and expanded the model, ensuring that more patients receive earlier interventions, some of whom will require surgery.
As with TAVR, the initial increase in surgical mitral and tricuspid valve replacement volumes is likely due to earlier identification of patients requiring surgical intervention. These surgeries will presumably decrease as alternative catheter-based procedures—many of which are now in clinical trials—become FDA-approved and commercially available.
Cardiac Transplantation and Mechanical Circulatory Support
Heart transplantation is also experiencing notable growth. Surgeons have performed record numbers of heart transplants in recent years—nearly 3,700 in 2020 alone. Even so, many patients remain on the heart transplant waitlist, necessitating the expansion of the donor population and advanced technologies in the area of mechanical circulatory support. Xenotransplantation and “heart in a box” are emerging as viable options for extending the distance an organ can successfully be transported. Both technologies are likely to increase volumes for cardiac surgeons specializing in transplantation.
Changing Complexity of Cardiovascular Surgery
As valve replacements and repairs migrate toward less-invasive alternatives, the remaining cardiac surgery cases are more complex and intensive, and often performed on patients with increased comorbidities. Between 2002 to 2016, the proportion of surgeries done in patients 80 years and older increased from 4.1% to 10.8%.While this population is not necessarily associated with a higher in-hospital mortality, they have a greater need for ICU-level care and tend to remain in the hospital longer than other patients. The median length of stay (LOS) for patients over 80 years was 9 days compared to 7 days for those under 80. As cardiac surgery cases increase in complexity, the field must prepare surgeons for this evolving demand.
Training the Next Generation
The future of cardiac surgery depends not only on emerging technologies, but also on surgeons’ ability to adapt their clinical training, which will require an increasingly integrated approach to fellowship and training programs.
More than a decade ago, vascular surgery began shifting away from open surgeries toward minimally invasive procedures, and today a graduating vascular surgery fellow may perform nearly 70% of their cases using catheter-based and less-invasive approaches.
Given the seemingly similar trends in cardiac surgery, the next generation of cardiac surgeons needs to be well positioned to deliver care using the most modern tools and approaches, including:
- Minimally invasive and percutaneous therapies, such as robotic-assisted percutaneous coronary intervention.
- Hybrid procedures, in partnership with cardiologists.
Similarly, future cardiac surgeons must remain at the forefront of technological advancements and participate in novel and highly complex procedures such as heart transplantation and xenotransplantation.
Positioning Your Cardiac Surgery Program for Success
The cardiac surgery landscape has shifted over the past decade. Lower-acuity cases are increasingly being performed with less-invasive alternatives to surgery, and technical advancements are expanding therapies to patients with advanced heart failure. The result is that cardiac surgeons are now managing more complex cases.
Looking to the future, CV program leaders should expect cardiac surgery to include:
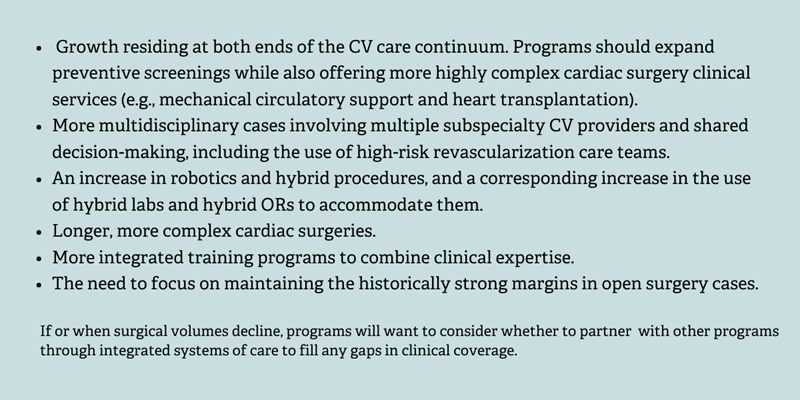
While cardiac surgery remains a crucial part of the overall CV service line, CV program leaders will need to consider their strategy to continue adapting to this ever-changing environment.
ECG’s cardiovascular consulting team is passionate about improving CV care delivery and since 2010 has conducted nearly 300 CV engagements across more than 100 parent companies. Our experts focus on providing executive advisory services to the nation’s leading CV programs.
Edited by: Matt Maslin

