In Brief: Hospital leaders are developing capacity command centers to address a multitude of frequent capacity and operational problems.
The term “command center” might conjure images of a dim, secure room, lit by the ambient glow of wall-size monitors, a team of headset-clad specialists delivering real-time data to an anxious director who paces back and forth, making snap decisions with life-or-death consequences—the stuff of suspense thrillers, not healthcare.
Hospital command centers are a bit less dramatic. But while they may lack the high profile of, say, NASA Mission Control or a counterintelligence operation, their core objective is the same—use technology to get the appropriate resources to the right place at the right time. And the decisions made within them can indeed be highly consequential.
What Is a Hospital Capacity Command Center?
Hospital capacity command centers (CCCs) are centralized hubs designed to manage patient throughput. They combine existing, traditionally siloed services or departments such as transfers, bed management, transport, and patient access, and put them under one roof—either physically, virtually, or in hybrid form. CCCs actively manage patient flow and supporting services, using real-time data and analytics to make decisions. They can have either a single-hospital, multihospital, or health system–wide scope, depending on the organization.
The past decade has seen the rapid expansion of CCCs. A 2022 national survey identified at least 25 health systems (out of 31 respondents) that currently operate CCCs, with an additional 5 actively planning to launch one.
Motivation for Starting CCCs
Hospital leaders develop CCCs to address a multitude of frequent capacity and operational problems.
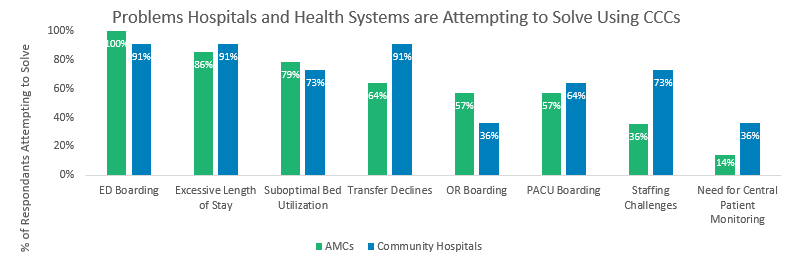
ED Boarding
Mitigating lengthy ED boarding time is the most common reason to build a CCC. Monitoring ED boarding involves tracking the number of patients waiting in the ED for an inpatient bed and the average wait time. ED boarders occupy treatment spaces needed for triaging incoming ED patients. Long boarding times can result in ED overcrowding, pose safety risks, and are associated with poor patient outcomes and longer length of stay (LOS). The Joint Commission consequently recommends aiming for a boarding time of four hours or less.
CCCs enable hospital administrators to take a dynamic approach to managing the number of patients boarding, discerning the clinical service(s) with the highest demand, and minimizing the wait time of patients with the most acute needs. CCCs can activate high-occupancy operational protocols that might include ambulance diversion, provider call, and requesting timely discharges from inpatient units.
Excessive LOS
Patients hospitalized for longer than expected based on their diagnosis take up beds, limit throughput, experience worse outcomes, and pose a risk for insurance denials. Health system leaders are using CCCs to reduce LOS by optimizing the patient journey, from admission to discharge and every step in between. Reducing overall LOS also improves ED boarding time and allows patients to be more quickly admitted to inpatient services where treatment can begin.
CCCs enable hospital operators to improve process time by optimizing the bed placement process, such as through close coordination between bed management and environmental services. Some CCCs engage case management and other clinicians in discharge barrier busting (e.g., interfacing across hospital departments to address waits for meds, DME, or tests) to reduce LOS of otherwise medically ready patients. These changes are possible because the central CCC:
- Has a view of the entire patient journey.
- Is empowered to make decisions to optimize patient flow.
- Has aligned incentives among support services to reduce LOS.
Suboptimal Bed Utilization
Health systems face varying capacity challenges across network hospitals. Frequently at tertiary or quaternary care facilities (i.e., hub hospitals or academic medical centers [AMCs]), the demand for beds exceeds the supply, creating constraints on patient flow. However, not all patients admitted to these sites require tertiary care capabilities. Smaller community hospitals may have available beds and the ability to care for these patients.
Administrators operating CCCs understand the long-term bed distribution of their health system and the capabilities of different hospitals. This facilitates faster transfers between levels of care and less time of patients waiting in “the wrong bed.” With a global view of capacity, CCC administrators can pinpoint specific needs for beds—for example, prompting ICUs to proactively identify patients ready for downgrade. Some hospitals may charge a physician in their CCC with overseeing ICU capacity and balancing ICU admissions from multiple sources—such as transfers and post-surgery cases—to best accommodate requests and minimize delays.
Transfer Declines
Hospitals are often forced to decline or delay transfers due to a lack of bed availability. This disrupts the continuity of patient care, causes frustration for referring providers, and risks revenue integrity.
CCCs balance internal system capacity with external transfer demand and focus on accepting and prioritizing patients the hospital can best serve (in line with correct levels of care, service offerings unique to hospital, and centers of excellence). Furthermore, other CCC efforts to monitor discharges and coordinate admissions increase system capacity, leading to the ability to accept more transfers. Streamlining the transfer acceptance process by optimizing the number of transfer acceptance pathways can also help manage and minimize transfer declines.
OR and PACU Boarding
OR and post-anesthesia care unit (PACU) boarding is a capacity challenge that AMCs in particular frequently cite as motivation for starting CCCs. PACU boarding occurs when patients hold in the PACU waiting for an inpatient bed (typically ICU level), and OR holds occur when patients wait in the OR due to lack of PACU beds being available.
Like suboptimal bed utilization, OR and PACU boarding results from mismatched time-of-bed availability. Surgical patients often “compete” with patients admitted from the ED for the same beds, and research has found that as much as 70% of ICU diversions are due to surgical volume variability. These delays are costly to hospitals and disrupt on-time start of subsequent cases.
CCCs monitor real-time and trended delays with these holds to address recurring and predictable challenges, adjust block scheduling or release, and request downgrades from ICUs to address upstream delays. A CCC physician can also oversee the triaging of patients between different ICUs (MICU, SICU, cardiac ICU, neuro ICU), as appropriate, to utilize excess capacity.
Staffing Challenges
Healthcare staffing shortages were a problem before the pandemic, and COVID-19 only exacerbated the issue. CCCs can’t fill vacancies, but through real-time monitoring of an entire hospital, they are positioned to deploy staff when and where they are needed most.
CCCs universally monitor bed availability and staffing to ensure the supply of hospital beds, and staff matches the current and predicted demand for beds as closely as possible. CCCs review data on demand for services such as transport and EVS and can deploy existing staff to maximize their impact (e.g., aligning shifts with timing of discharges). CCCs often incorporate nursing float pool administration, further streamlining the deployment of staff across the system where needed.
Need for Central Patient Monitoring
CCCs can offer a more economical way for smaller community hospitals to incorporate central patient monitoring (e.g., fall monitoring via video or sepsis monitoring via a live feed of clinical information) through a centralized enterprise service. Additional central patient-monitoring services being incorporated into some CCCs include tele-sitter services, virtual ICUs, and hospital at home. These one-to-many approaches provide scalability, cost efficiency, and increased patient access. The CCC’s system-level view improves its ability to deploy these services where they’re needed most.
How to Build or Grow a CCC
CCCs are as varied and complex as the variety of drivers that spur their development. While there are common reasons for why health systems develop CCCs, the departments differ in function, governance, and scope (e.g., hospital or health system).
If your hospital or health system is considering a new or expanded CCC, check out our recent article in the Joint Commission Journal on Quality and Patient Safety, written in conjunction with the Hospital Capacity Management Consortium, an industry work group for capacity management with the goal of improving the efficiency of acute care capacity management. Finally, ECG’s team of capacity management experts can help your system navigate starting, evaluating, or expanding your CCC.
It’s time to improve the efficiency of acute care and capacity management.
Is your hospital or health system considering a new or expanded CCC?
Edited by: Matt Maslin

