
Like most health systems, Mid-America pays its doctors using an RVU-based system that has functioned fairly well for the past 5 years – compensation is market-competitive, physicians understand their productivity expectations, and financial investments in the physician group are reasonable and justifiable. However, the payer environment is beginning to change. Mid-America has launched a medical home pilot, plans to participate in the Medicare ACO, and is working with several commercial payers to design bundled payments for high-cost episodes, all as the new Medicare DRG weight reductions are looming. In addition, patients are increasingly using e-visits through Mid- America’s electronic health record and patient portal. As a result, physicians have started to both complain about “uncompensated care” related to e-visits and ask for “replacement” RVUs.
Physician group executives are wondering: Is now the time to change the compensation program to incentivize the outcomes needed to succeed in a value-based reimbursement environment? Over the past 10 years, most hospitals and health systems have adopted and managed RVU-based compensation systems for their employed physicians. These models were necessary and functioned well following an era of large-scale losses on physician groups, which were partially fueled by high levels of guaranteed compensation and misaligned incentives. The models were particularly adept at incentivizing physicians to see a reasonable number of patients per day, which helped to offset practice overhead and staffing. A direct consequence of this was a built-in incentive to generate face-to-face visits, procedures, and ancillary testing to maximize compensation in these systems. But as reimbursement shifts, how should organizations be thinking about incentivizing physicians when volume is not the only driver of reimbursement? What about incentives for managing the complex diabetic patient? Or for keeping the patient with multiple chronic conditions out of the emergency department (ED)? Or avoiding readmissions? More forward-thinking organizations are beginning to migrate quality- and other value-based measures into compensation plans. There are several keys to making these plans work:
- Acknowledging that volume still matters.
- Finding smarter, more efficient ways for providers (e.g., physicians, RNs, MAs, case managers) to collectively manage their patients’ health (e.g., e-visits, group visits, patient-provider e-mail, telephone consults).
- Investing in the infrastructure to measure and act upon quality and outcomes.
- Pursuing contracting/managed care reimbursement models that reward similar outcomes to those in the compensation plan.
Organizations that are not ready to aggressively shift their managed care payment structures are better off maintaining their pay-for-volume compensation plans in the short term. However, these organizations should also be introducing quality metrics, even if they are not tied to financial incentives in the immediate term. For those organizations embracing a pay-for-value contracting strategy, augmenting physician compensation incentives is imperative to achieving outcomes that are tied to new reimbursement contracts.
Can Panel Size Be the New Productivity Measure for Primary Care Physicians?
Panel size is an often-cited but elusive metric that measures different things in different organizations. Those organizations that have significant capitated populations or operate in PCMH models are likely to have attribution methodologies and internal standards for distributing patients. However, at this time, there are no reputable publicly available sources of panel size benchmarks to use in compensation planning, and it is likely that even if benchmarks were available, the calculation methodologies would be significantly different and would largely prevent an apples-to-apples comparison. Still, while the market data is catching up, panel size can be an effective tool for comparing physicians intraorganizationally and illustrating why volume still matters. If you compare two physicians, one who is managing 2,000 patients and one who is managing 1,000 patients, both with the same quality scores, utilization profiles, and patient experience ratings, the physician managing more patients is clearly of higher value to the organization.
Case Study: Methodologies to Pay for Panel Size and Quality
In keeping with the theme that volume still matters, a point-based value system can be developed to differentially reward quality for those with larger panels. This system can be incorporated into current pay practices, used as a replacement methodology, or phased in at greater percentages over time. High-level steps involved in developing such a system include:
1. Define panel size attribution methodology.
2. Examine internal variation in panel size.
3. Set panel size parameters/targets.
4. Determine desired quality measures (e.g., diabetes bundle).
5. Develop targets for desired measures.
6. Develop a point-based system to reward those physicians meeting the quality target for the entire panel, as well as the number of
patients for whom the measure applied and the care intervention that was performed, in order to weight quality performance based
on panel size.
7. Review results for providers and adjust point allocations as necessary.
8. Determine magnitude of incentive and how it fits into your overall compensation structure.
During a recent client project, ECG Management Consultants developed a point-based incentive system to reward performance on 14 HEDIS measures across adult primary care physicians (PCPs) with a definable panel. Those PCPs who had larger panels and high quality scores earned differentially more points than those who had smaller panels and did similarly well on quality measures. Accordingly, those in the highest quadrant (large panel, high quality) received the largest incentive/compensation payment.
There are several ways to begin the process of incorporating quality-based features into your provider compensation plans. Strategies to consider include:
- Establishing a base salary at a percentage of market (e.g., 80 percent of median) with a more robust quality incentive (i.e., 20 percent or greater).
- Moving completely to a panel- and quality-based incentive system for clinicians operating with defined panels (e.g., PCMH, significant capitated lives).
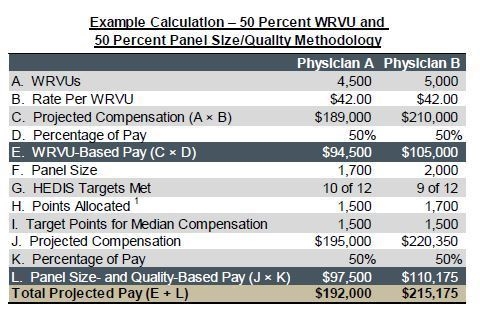
- Running parallel plans, weighted based on the organization’s contracting strategy (e.g., 40 percent WRVUs, 60 percent panel size). Sample plan calculations are illustrated in the table.
The Decision: Moving Your Employed Physicians to Value-Based Compensation
While not every physician organization is ready to disrupt its fee-for-service (FFS) physician compensation programs in favor of something more panel- and quality-based, at some point soon, enough revenue will be based on non-FFS performance measures that changing physician incentives will make sense from a patient care perspective and a financial one. A compensation program similar to the one described here can be used in conjunction with traditional FFS (RVU) pay or with some level of base salary combined with the point-based value system. Increasingly, we are seeing that PCPs are amenable to being paid differently, and organizations are starting to align new reimbursement incentives with their compensation plans.

