
Impact of Reform
Under the ACA, funding for FQHCs is increased by $11 billion1 specifically for the expansion of primary care services for all patients and provision of a medical home for uninsured patients. FQHCs continue to receive cost-based reimbursement from Medicare and state-specific prospective payments or contracted managed care rates from Medicaid and will likely receive depressed commercial rates for exchange-based contracts. Additionally, FQHCs receive earmarked state, federal, and local grants to treat uninsured patients.
FQHC Overview
FQHCs were established to improve community health, particularly among vulnerable and underserved populations. The FQHC serves residents of the center’s designated shortage area or all individuals within an FQHC’s designated special population, providing primary care, diagnostic, and preventive clinical services. FQHCs also provide case management (CM), enabling services such as outreach, transportation, and education regarding the availability and proper use of healthcare services.
Unlike most providers, FQHCs are considered a safe harbor from the Anti-Kickback Statute,2 provided that arrangements are not conditioned upon referrals to the supplier. Appropriate arrangements result in savings of federal grant funds or increased revenues to the FQHC, do not limit patient choice, protect the independent medical judgment of providers, and can reasonably be expected to maintain or increase service availability or quality. Special protections are also granted to services provided by FQHCs via the Federal Tort Claims Act, which deems FQHCs, employees, and eligible contractors to be employees of the federal government, thus requiring malpractice suits to be filed against the federal government.3 This eliminates the need for malpractice insurance for services rendered by providers as part of contracts with FQHCs.
Partnership Strategies
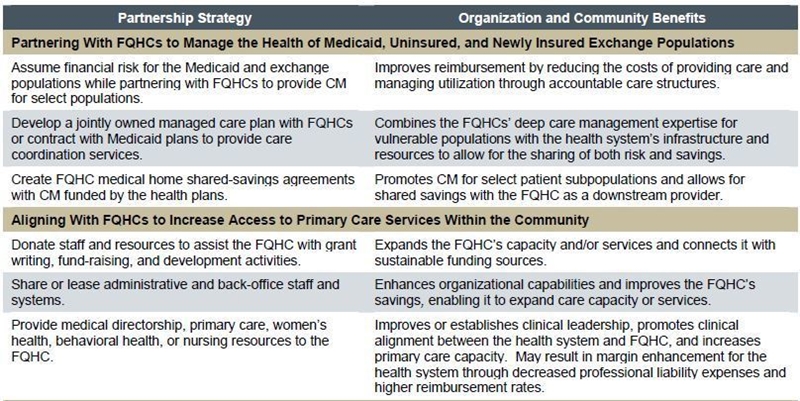
Building relationships with FQHCs can enable health systems to improve the value, availability, and appropriateness of care for all members of the community. As reimbursement moves toward increasingly risk- and value-based models, FQHCs are also uniquely expert providers within the continuum of care for patients at higher risk for avoidable care due to socioeconomic and clinical factors. Successful partnerships between health systems and FQHCs focus on collaborative strategies of mutual and community benefit. Overarching strategies leading to benefits for all parties may include:
- Partnering with FQHCs to manage the health of Medicaid, uninsured, and newly insured exchange populations.
- Aligning with FQHCs to increase access to primary care services within the community.
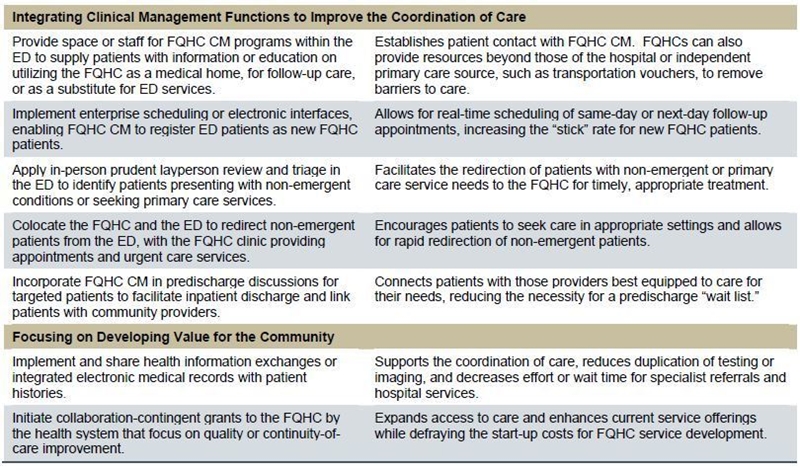
- Integrating clinical management functions to improve the coordination of care.
- Focusing on developing value for the community.
Footnotes
1. The Henry J. Kaiser Family Foundation, Focus on Health Reform: Summary of New Health Reform Law, April 19, 2011.
2. 42 CFR § 1001.
3. 42 USC 216 and 42 USC 224, 60 FR 22530.

