
The relationship between a hospital/health system and its medical school/university partner is typically codified in an affiliation agreement. These documents define the business terms that guide participants’ collaborative involvement in educational, research, and clinical activities. While managerial authorities, participant responsibilities, and transactional clarity are fundamental to any affiliation agreement, it is the structure and design of the affiliation governance model that is most predictive of the participants’ ability to successfully advance the partnership in the future. Inevitably, a productive strategic affiliation creates opportunities for both parties to gain access to competencies and resources that enable them to enhance/expand their individual and collective enterprises in ways that would not be possible independently.
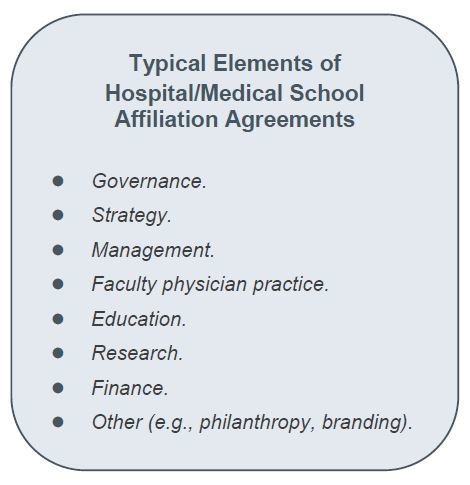
Despite the consequential nature of these documents, a random sample of existing affiliation agreements from across the country would reveal wide variation and an array of topics covered in these often extensively detailed arrangements. For example, affiliation agreements commonly address the parties’ expectations and responsibilities for medical student clerkships and graduate medical education. They might also define the locus of policies and accountability for the conduct of research by faculty, residents, and students in the clinical environment. Some agreements attend to topics of faculty physician practice and the reciprocity of hospital medical staff and medical school/university faculty appointments. They may also address the alignment of medical school academic leadership positions with hospital service line and medical staff leadership positions. Invariably, hospital/medical school affiliation agreements define financial arrangements, funds flow amounts, and the related terms and fiscal processes agreed to by the parties.
Unfortunately, it is not uncommon for those entities participating in affiliation agreements to devote little attention to the governance construct of the affiliation and, thereby, to how strategy can be collaboratively determined and pursued. In fact, the most transactionally focused affiliation agreements are often silent on the topic of governance, or governance of the relationship defaults to those managerial point persons with administrative responsibility for the agreement. Governance arrangements of this type between hospitals/health systems and medical schools/universities arguably create significant strategic and other risks for the participants. For example, it is highly likely that most clinical-academic affiliations will be challenged over time by dynamic circumstances and events that might have been unforeseen or unknown at the time the affiliation agreement was executed. Examples of such circumstances might involve:
- Competitive physician recruitments/programmatic opportunities.
- Emergence of new clinical/academic partners and/or competitors.
- Disputes arising from unintentional clash of strategies or initiatives.
- Redundant or incompatible investments and/or financial plans.
While the specific challenges to the affiliation may not be predictable, the need for a governance model that is grounded in trust and fosters meaningful communication to address such circumstances when they do arise is essential.
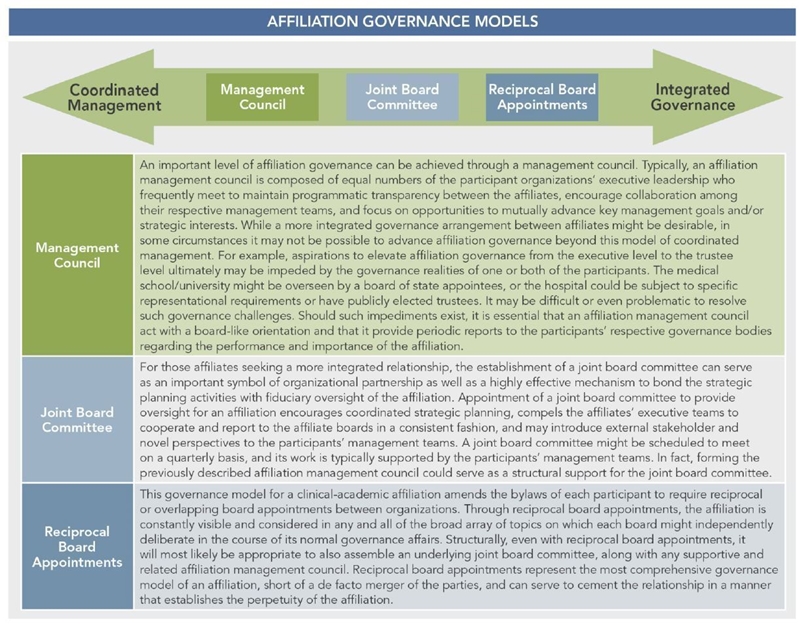
More mature and contemporary affiliation agreements establish well-conceived governance constructs that enhance the participants’ relationship, provide a framework for addressing inevitable disputes, promote cooperative planning processes, and thereby foster and convey strategic benefit. Accordingly, the design of an effective governance model for a hospital/medical school affiliation is fundamental to realizing the potential of the partnership and ensuring its longevity. While there are a wide variety of possible governance arrangements for hospital/medical school affiliation, each is often reflective of the unique organizational characteristics and imperatives of the participants. The graphic below depicts the range of affiliation governance paradigms.
Conclusion
Engagement in a hospital/medical school affiliation represents a highly strategic decision by the participants to mutually leverage complementary assets and interests and gain access to an expanded set of competencies and/or resources. For the parties to avail themselves of the full strategic benefits of such an alliance, careful consideration must be given to the design and construct of the affiliation governance relationship. It is only through an effective affiliation governance model that the strategic importance of elevating the status and success of each affiliate partner becomes a mutual paramount concern.

