
Let’s be honest. Although the meaningful use (MU) criteria in Stage 1 of the Electronic Health Record (EHR) Incentive Program may have been challenging on many fronts, they did not require significant change on behalf of your eligible professionals if the practice had previously implemented an EHR. The requirements reinforced routine and ongoing activities. For example, standing protocols may have already included entry of demographics and basic vital signs; maintenance of allergy, medication, and problem lists; and e-prescribing. New processes, such as smoking status capture for specialty practices and the provision of clinical summaries, mostly became the responsibility of the front desk and clinical support staff. The Stage 2 criteria, on the other hand, require an expanded level of system adoption by eligible professionals that can’t as easily be avoided through delegation. This article addresses the potential redesign of the clinical process to better ensure your organization’s full funding in light of Stage 2 of MU.
Providers that attested for Stage 1 beginning in 2011 or 2012 must meet the Stage 2 requirements during any 90-day period in 2014. If the first year of Stage 1 attestation is in 2013 or after, the provider has to meet the Stage 2 requirements by the beginning of their third calendar year in the program. For instance, if a provider attests for Stage 1 in 2014, they must begin reporting on the Stage 2 requirements by January 1, 2016. With an understanding of how they will need to interact with their patients, other providers and care teams, and technology, providers and their operational leaders can focus on a few key initiatives that will help position them for a smooth transition into the next stage of MU. Focusing on these high-level initiatives will help position your organization for success as you work to meet the various Stage 2 criteria.
Interaction: Provider to EHR
Stage 1 criteria allow for minimal adoption of the EHR, especially when providers are surrounded by competent support staff. Stage 2 outlines specific criteria that will force providers to start using the EHR on a more direct level. As a core measure, computerized physician order entry (CPOE) is now required for a minimum of 60% of medications and 30% each of laboratory and radiology orders. Following the Stage 1 requirements, the Centers for Medicare & Medicaid Services (CMS) relaxed the rule to allow certain staff members (i.e., medical assistants) to place orders using the EHR. In most cases, however, it will be more efficient for the provider to prescribe medication and order laboratory or radiology tests in real time so patients can fulfill those orders as soon as they leave the office. The goal with the increased CPOE threshold is to help employ the use of clinical decision support (CDS) tools at the point of order entry, which CMS states will lead to increased patient safety and quality of care.
A study by the Institute of Medicine estimates that 98,000 deaths are caused by medical errors in the United States – EHRs are designed to contain alerts to help decrease that number. However, providers need to keep in mind that an EHR’s built-in CDS tools will only work if the system is used as it is designed. A medical assistant presented with an alert for a contraindicated medication or test is unlikely to be able to make an informed decision to override the alert or accept an alternate suggestion; the provider, however, can appropriately choose the best option for the patient without delay if he/she is the one placing the order. Those providers who in the past delegated the majority of these tasks to others are going to be less able to do so as they move from Stage 1 to Stage 2 of MU. That being said, it is more important than ever that activities that can appropriately be performed by midlevel providers, nurses, and medical assistants be delegated accordingly so that physicians can focus on those tasks that require greater knowledge and expertise.
Interaction: Provider to Patient
Patients have long taken a back seat in the management of their healthcare, and for understandable reasons. In many cases, barriers used to exist that delayed the process of patients obtaining access to their personal health records. Various obstacles, such as lengthy paperwork, organizational processes, and HIPAA requirements, all played a role. Most patients believed that the added benefit wasn’t worth the hassle, especially if they couldn’t make sense of the lab results or various diagnoses. With Stage 2 criteria comes a mandate for physicians to increase patient access to online medical records through patient portals and to provide patient reminders and educational materials in the same manner. Quicker turnaround time has also been applied in some cases, for example, when providing clinical summaries or entering discrete data into the system (to increase real-time CDS capabilities). According to a study from Manhattan Research, LLC, 50% of the general patient population would consider switching providers in order to have online access to their medical records. Along the same lines, a patient’s ability to communicate with his/her practice via secure messaging is central to one of the new core measures in Stage 2. When properly managed, patient knowledge is a good thing – it can translate into compliance with recommended preventive care measures, fewer hospital readmissions, more accurate clinical decisions, and more targeted diagnostic testing on the part of the physicians and practice staff.
Interaction: Provider to Provider/Care Team
Finally, eligible professionals will be required to satisfy 17 core measures under Stage 2 rules. Outlined in the new criteria are measures that encourage provider interaction with other providers, entities, and care teams. Specifically, three of the Stage 1 menu set items that directly affect provider/provider interaction were upgraded to core objective status under the Stage 2 rules. First, providers will be required to provide summary-of-care documents for more than 50% of transitions of care and referrals, with 10% being transmitted electronically. Second, medication reconciliation must be performed for at least 50% of transitions of care. Third, providers must demonstrate their ability to submit electronic data to immunization registries/systems on an ongoing basis. As health systems become more and more connected, the need to increase related lines of communication becomes more apparent. Accordingly, as provider/provider communication increases, organizations can begin to improve population health while eliminating some of the unnecessary waste that currently exists in the industry, such as duplicate or otherwise unnecessary tests.
So What? Now What?
How do these new requirements affect providers? Aside from understanding the technical variations that will change as they move from one stage to the other, successful adoption of Stage 2 criteria will require significant operational efforts to ensure that day-to-day activities do not become unnecessarily cumbersome, which is a likely outcome if the new MU requirements are layered onto existing work flows instead of incorporated into an entirely redesigned clinical process.
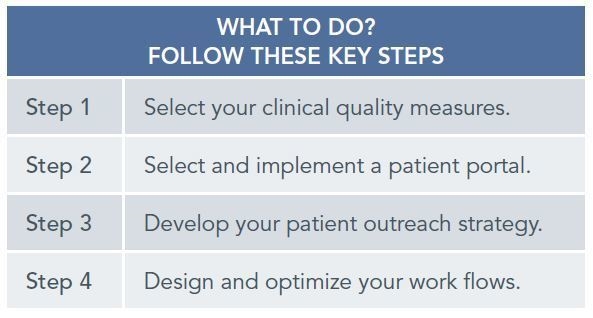
We have outlined four steps that organizations can take to help define the requirements to succeed, plan for the elements necessary to meet Stage 2 requirements, and ensure that the appropriate processes are in place to allow providers and their teams to continue providing high-quality care. Although there may be other initiatives organizations can undertake to help prepare for future requirements, these four steps are essential to laying the foundation to help you move forward into the next stage of MU and will help prepare you for future quality and patient engagement projects.
Step 1: Select Your Clinical Quality Measures
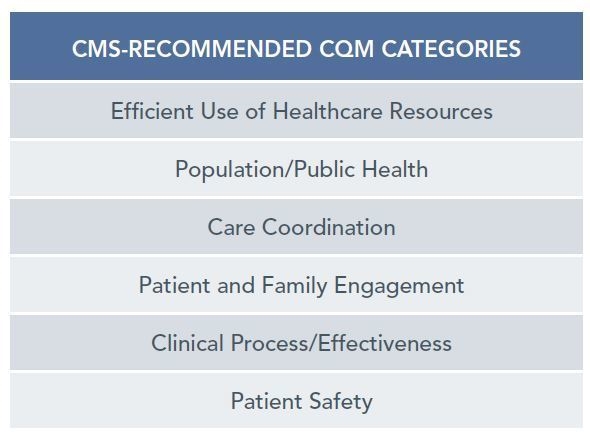
As a standard, decide what will drive your organization’s adoption of Stage 2 criteria. Beginning in 2014, eligible professionals will be required to report on 9 of 64 clinical quality measures (CQMs). CMS has recommended six key measures for eligible professionals but gives provider organizations the flexibility to choose from many. Whichever CQMs you decide to use, choose those that fit your operational goals and support your vision for the future. As you decide what direction to take, ensure the right people are involved in the decision-making process, understand how reporting on those items will change your current processes and work flows, and communicate to your audience (e.g., providers, staff, patients) your plans for implementing any necessary changes. If you have an existing quality program, define and focus on the CQMs that will help you meet your program’s mission. If you don’t, now is the time to put a program in place; you will have a unique opportunity to establish the initiative from the ground up. Having a solid plan in place for your clinical quality initiatives will not only help you meet the Stage 2 criteria but will also help inform other activities as you increase adoption of your EHR.
Step 2: Select and Implement a Patient Portal
Increasingly, patients cite their ability to communicate online with their health professionals as central to their decision in choosing a provider. Stage 2 outlines two specific core measures that require eligible professionals to offer a tool for patients to access their health information online. Understandably, provider organizations have implemented, or are considering the implementation of, a patient portal that integrates with the EHR that is currently in place. However, it is important to note that functionality among existing patient portals varies to a great degree. Before selecting a tool, identify the features that are most important in managing your patient population online. While some EHR vendors offer a product that is built into their ambulatory software, there are other alternatives available on the market that may better suit the identified needs. Think about what features you would use and, more importantly, what your patients are asking for, such as online bill pay functionality or integration with health insurance plans. As more patients manage their health online, products will evolve and offer better features. At a minimum, choose a product that will meet the needs of your patients now and in the future. Once a tool is chosen, identify and involve various stakeholders and teams to help you think through your implementation strategy. Understanding the functionality, as well as the needs of your providers and patient population, will help you achieve greater rates of adoption upon implementation of the portal. Keep in mind that the most successful implementation projects require months of planning, design, and communication to all parties affected – providers and patients alike.
Step 3: Develop Your Patient Outreach Strategy
In conjunction with your portal strategy, think about how you will engage and stay connected with your patients, as the onus of meeting the Stage 2 criteria lies only partially on the providers’ use of the system. For example, patients must successfully demonstrate use of the portal, too, and your providers are responsible for encouraging the two-way communication. Elements to consider when developing your patient outreach strategy include the need to send patient reminders for appointments and health maintenance items, how you would like to present patients with educational materials (e.g., online preventive health sessions), and what standardized communication protocols will be put into place across the organization. Think about how you will encourage patients to take ownership of their health. Online education tools that integrate with EHR systems can provide timely information to your patients to help them understand how to manage disease, pre- and post-operative instructions, or general information regarding a diagnosis. Mobile apps and Web tools can drive patients to your physician population when it is necessary to seek in-office advice. Patient-directed surveys will not only help your organization understand how to improve but will reassure your patients that you are taking a proactive role in the management of their health. Conventional methods still work, too. Visibility in the community, follow-up telephone calls, and, believe it or not, snail mail, are all realistic options to engage your patient population.
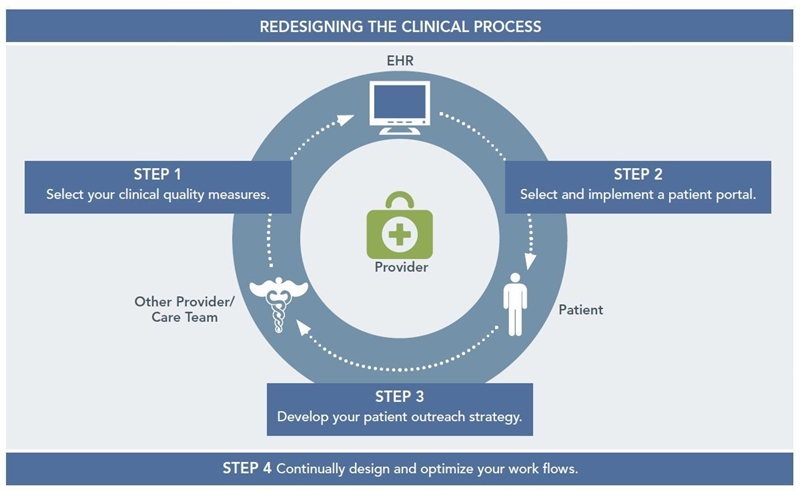
Step 4: Design and Optimize Your Work Flows
There is no doubt your work flows have changed since implementing an EHR. Like any practice, there are growing pains associated with a change to learned behaviors, so it is natural to have concern over the additional criteria required by Stage 2. Rather than viewing these criteria as a burden, providers should use this opportunity to understand what is working well and what needs improvement, and to map out where new processes required by Stage 2 will affect the business. Once the requirements are identified and understood, define precisely how you are going to address the changes moving forward. For instance, how are you going to address patient questions submitted through the portal? What will your process be to ensure that your patients’ conditions are communicated to others on associated care teams? Your work flows should be revisited often, especially in today’s quickly changing healthcare environment. While inefficient processes can frustrate staff, block access to patient care, and leave revenue opportunities on the table, a well-executed plan will have the opposite effect and help your practice flourish – even in the face of mandated regulatory change.
React and Interact
The 672-page document from CMS that provides the final criteria to meet MU Stage 2 requirements can be a little overwhelming. The rules, however, are straightforward. If you are already on the right track and just need to understand what variations exist from Stage 1 to Stage 2, don’t neglect the planning, operational, and messaging needs that will support the changes, no matter how small they may seem. If you are behind the curve and still using the EHR as little more than an electronic chart, you first need to understand what will help you begin using the EHR the way it was intended – as a tool to provide better care. In every case, all healthcare professionals should maintain or refocus on collaboration among their colleagues and care teams. Finally, it will be critical to open the lines of communication with patients; they and their health are depending on it.

