
The economics of private practice are becoming increasingly complex and daunting as reimbursement models shift in conjunction with healthcare reform. In response to ongoing change, hospitals and healthcare provider organizations are seeking stability and security in the form of highly integrated arrangements that formally align hospitals and physicians. Comanagement is emerging as a popular alignment option with the potential to increase physician participation in service line decision making while strengthening performance, quality, and leadership.
Though hospital/physician alignment is a popular topic of conversation and the adoption of comanagement strategies is growing more prevalent, many physicians and health system administrators lack a complete understanding of key facets of the structure, development, and implementation of these arrangements. This article is the first in a two-part series; it explores the rationale behind comanagement strategies and highlights essential structures necessary for the development of these agreements. The second piece in the series, entitled “Operationalizing Your Comanagement Arrangement,” provides an overview of the key steps involved in the implementation of comanagement agreements, as well as some of the common pitfalls to avoid.
The Impetus for Comanagement
Under a typical comanagement arrangement, hospitals or health systems contract with independent community physicians to oversee day-to-day operations and conduct long-term planning for a specified service line. Among the most frequently comanaged service lines are cardiology, orthopedics, and oncology, due to their strategic importance and the scale of opportunity for improvement under physician management.
By sharing both management and financial responsibilities through a comanagement model, the goals of the hospital and physicians can be aligned to enhance care delivery and quality within the service line, while also facilitating the development of new service line opportunities. The most successful of these arrangements are borne out of a clear understanding of the rationale behind these strategies and the benefits to each participant in the arrangement.
Comanagement arrangements have the potential to increase physician participation in service line decision making while strengthening performance, quality, and leadership.
Hospital/Health System Rationale
In general, a comanagement agreement provides an opportunity to increase physician participation in decision making, improve the patient care experience, and enhance the operational and financial reporting capabilities of a service line. While these benefits can be accomplished through employment, physicians in key specialties are often fiercely independent and averse to employment discussions. Further, many hospitals are increasingly discovering that employing specialists is exceedingly expensive, and thus are seeking alternative methods for alignment.
From the perspective of hospitals, comanagement offers a cost-effective and collaborative alternative for the integration of these specialists. The enhanced integration provided through a well-designed arrangement establishes a direct line of input from physicians into service line growth strategies, quality initiatives, and performance improvement ideas. The comanagement planning process alone can foster the development of tools and mechanisms to promote physician attention to quality, service, and development issues.
When successful, the execution of a comanagement arrangement has the potential to alleviate mistrust between physicians and hospital administration and to lay the groundwork for future integration efforts (possibly including employment or other initiatives).
Independent Physician Rationale
Physicians are increasingly interested in aligning with hospitals for a variety of reasons, including mitigating a declining revenue base. Comanagement is one of a few models that provide economic benefit to physicians while also allowing them to preserve practice independence (physician professional billing practices are generally not impacted). Such an arrangement also provides physicians with greater influence over hospital operations, which can enhance efficiency and physician satisfaction.
Healthcare Reform Perspectives
As reimbursement is increasingly tied to performance and the coordination of care for both physicians and hospitals, the comanagement model may serve as a tool to jointly improve care delivery and enhance value. This is particularly true for health systems engaged in value-based purchasing and risk-sharing/ACO models for which reimbursement is tied to specific performance metrics. Comanagement compensation mechanisms can be designed to align physician incentives and improve performance, positively impacting both technical and professional revenue.
Comanagement Model Overview
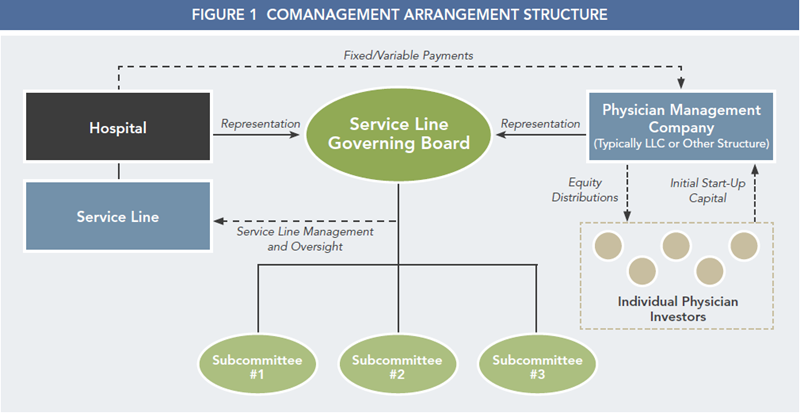
Under a comanagement agreement, participating physicians are compensated to oversee the management of a distinct hospital service line through fixed payments for base management services and incentive payments contingent on performance. In our experience, the specific details of comanagement agreements differ widely across hospitals and specialties. Although the goals are the same, a high degree of creativity is frequently utilized in designing these arrangements to reflect the unique needs of hospitals, physicians, and patients. With that said, these agreements generally have a foundational structure, as outlined in Figure 1, and also encompass similar considerations for service line performance, compensation, governance, and management structures.
Scope of Services
In the absence of a defined service line strategy, physicians frequently act primarily in the interest of their independent practice, even to the point of sometimes paying little attention to overall hospital service line quality, service, and costs. Comanagement agreements provide the opportunity to change that unfortunate reality by paying physicians to enhance performance through the following activities, among others:
- Providing physician leadership over the service line, frequently working in a dyad with the service line administrator.
- Providing input pertaining to the hiring and managing of nonphysician clinical employees.
- Assisting the hospital in implementing, monitoring, and managing quality assurance and utilization review activities.
- Developing, implementing, and regularly updating patient care (clinical) protocols, pathways, and guidelines.
- Assisting the hospital in the management of supply chain activities and the purchasing/leasing of medical equipment, and actively seeking methods to control costs.
Compensation
Although compensation mechanisms vary widely across the spectrum of comanagement agreements, both fixed and variable compensation components are universally included.
The fixed portion of compensation is a payment made based on an hourly rate for documented physician time spent on medical directorship duties or committee participation. This portion must comply with fair market value (FMV) principles and typically represents approximately half of the total potential payment. Due to the overlap in services provided, any existing medical directors or service line administrators should be compensated as an expense from this base management fee.
The variable portion consists of performance incentives paid based on achieving specific quality, operational, and financial goals. The total amount of incentive compensation must be determined in advance of a contract year, and achievement should at least reflect an improvement over current performance, if not a high level of performance compared to available industry benchmarks. While there is substantial room for flexibility in the design of the performance goals, from a legal standpoint, metrics should not directly link to patient volume or length-of-stay measures.
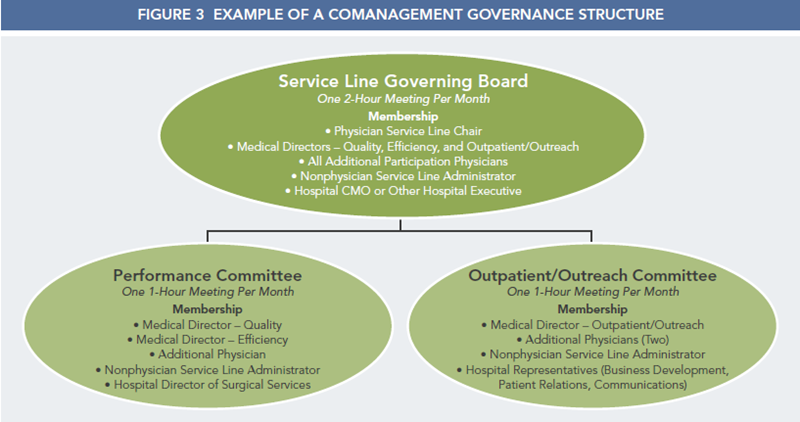
Service Line Governing Board
The governing board (or similar leadership body) generally acts as a strategic planning committee and decision-making body for the service line. With representation from both the hospital and participating physicians, the board’s responsibilities typically include (but are not limited to):
- Developing the service line plan and monitoring management company performance.
- Reviewing clinical quality and the overall performance of the service line.
- Developing recommendations in regard to the annual budget.
- Reviewing arrangement payouts and adjustments.
For larger service lines, it is common to form additional committees to support the board through more frequent monitoring and facilitation of specific agreement components. These committees would also include joint representation from both the hospital and participating physicians. Example committee activities include:
- Establishing baseline performance and developing relevant reports.
- Monitoring incentive metric performance.
- Addressing opportunities and concerns related to patient access.
- Planning and overseeing the execution of outreach and marketing initiatives.
- Addressing the development and maintenance of relationships with community physicians.
A sample governance structure that might be utilized in a comanagement agreement is provided in Figure 3.
Management Company
The arrangement typically involves creating a new management company composed entirely of physicians, although in some cases hospitals contract with an existing physician group or with multiple individual physicians. In most arrangements, the management company established is solely a legal entity without a dedicated facility, equipment, or staff. The management company provides administrative rather than clinical services, and physicians continue to see patients and bill payers through their medical groups. A small capital contribution is required from physicians to pay legal and other fees required to establish the corporation and pay minimal operational fees moving forward. One of the advantages of the management company framework is that physicians have the freedom to develop their own mechanisms for distributing compensation within the group. The distribution methodology can be designed to reward arrangement leadership and time invested, but it cannot be based on the value or volume of physician referrals/business generated for the hospital.
Strengthen Service Line Performance
When designed appropriately, comanagement arrangements are a cost-effective way to better engage physicians in the improvement of hospital services while allowing them to maintain practice independence. Given the potentially complex design and high reward of these arrangements, it is important to execute an inclusive and organized planning process to increase the probability of successful implementation. With the right case for development in mind and the proper components in place, comanagement arrangements represent an opportunity to significantly strengthen service line performance, quality, and leadership.

