
During the last decade, state Medicaid agencies have embraced managed care as the predominant delivery system. In addition to the goals of reducing cost and improving clinical outcomes, states are looking to more efficiently and effectively deliver care to the roughly 21.3 million additional Americans who could be insured through the Affordable Care Act’s (ACA) Medicaid expansion.1 While states share a number of common objectives, each state also employs a unique approach to managed care and an individualized mix of innovation and quality improvement tactics. These innovative Medicaid managed care models are driving healthcare transformation and, in conjunction with federal incentives, are leading to effective care delivery modalities that may very well extend beyond Medicaid.
This article summarizes the increasingly prevalent Medicaid managed care model to help inform providers’ strategies for serving Medicaid patients. It also presents real solutions for addressing some of the key challenges organizations face in managing their Medicaid members.
HISTORY OF MEDICAID MANAGED CARE
Medicaid managed care delivery systems grew rapidly during the 1990s. In 1991, 2.7 million beneficiaries were enrolled in some form of managed care. Currently, managed care is the most common Medicaid delivery system, with all states except Alaska and Wyoming having all or a portion of their Medicaid population enrolled in managed care programs, covering more than 50 million recipients nationally.2
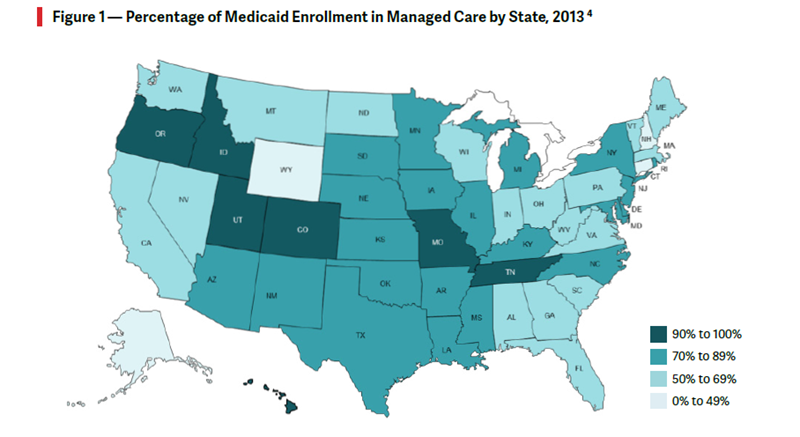
Of the 39 states (including Washington, D.C.) with managed care organizations (MCOs), more than 75% of the Medicaid population is enrolled in an MCO, and more than half of these states have expanded Medicaid managed care in the last 2 years by adding new eligibility groups, mandating managed care enrollment, and/ or expanding MCO coverage to new geographies.3 As seen in Figure 1, by 2013, seven states had over 90% of their Medicaid population enrolled in MCOs. Since then, six more states have moved to enroll over 90% of their population in managed care.
States have been motivated to move to managed care primarily to control costs, but the expanded availability of federal funding has provided an added incentive. The State Innovation Models (SIM) Initiative and the Medicaid Innovation Accelerator Program (IAP) are two federally funded initiatives created to help states overcome the financial burden of implementing innovative infrastructure to support healthcare transformation. Under the SIM program, awarded states have received nearly $1 billion from CMMI to test innovative delivery models and build infrastructure to support the movement of Medicaid populations to managed care more quickly. The IAP program complements these efforts and provides additional federal support and tools for improved data integration, quality measurement, peer-to-peer learning, and spreading lessons learned.
INNOVATION STIMULUS
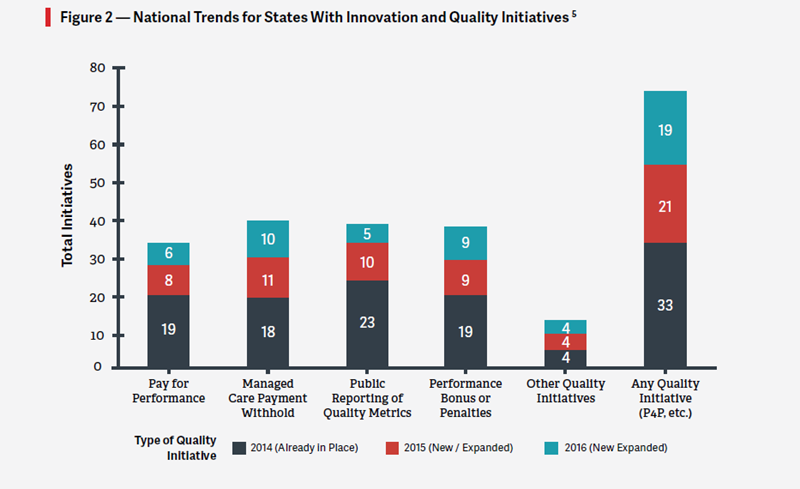
Medicaid MCOs typically perform care management and coordination functions as part of their state contracts, with the goal of funding these activities using the expected savings from reductions in unnecessary hospitalizations, ER use, and other costly services, and through effective management of patients with chronic conditions via primary care provider accountabilities. Medicaid care coordination strategies include health homes, patient-centered medical homes (PCMHs), accountable care organizations (ACOs), and the integration of behavioral health into primary care. All of these initiatives rely on technologies to create greater clinical integration between providers, facilitate patient engagement, and standardize care delivery. These initiatives are becoming increasingly prevalent as part of each state’s approach to managed care, as seen in Figure 2, with varying degrees of success toward achieving savings.
CHALLENGES AND SOLUTIONS FOR MEDICAID MANAGED CARE
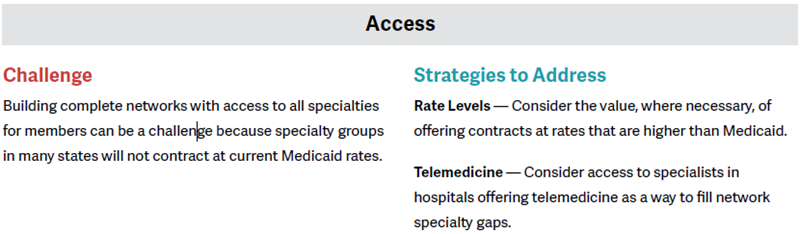
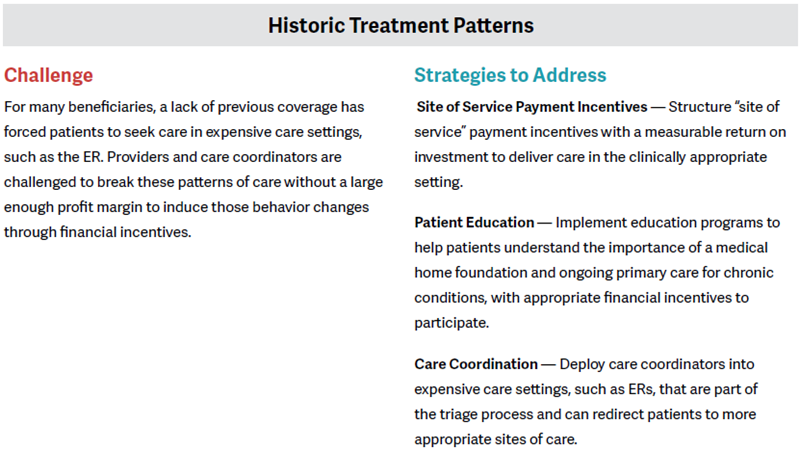
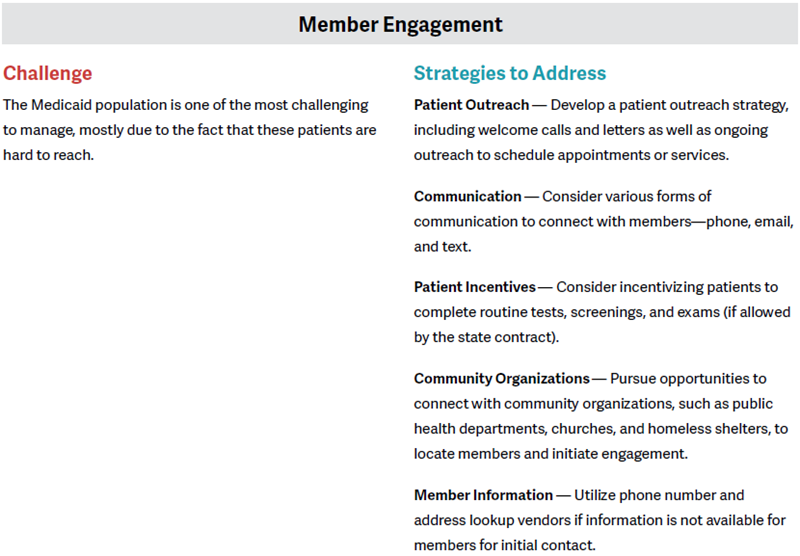
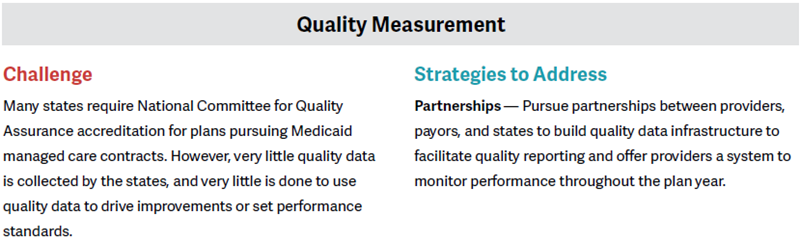
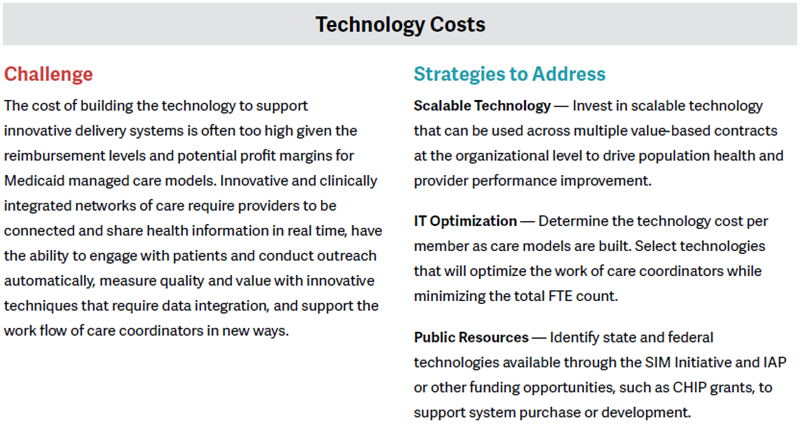
Although the federal and state governing bodies continue to emphasize improving and expanding Medicaid coverage, research continues to highlight the various challenges and gaps in Medicaid managed care efforts. Given that Medicaid currently covers about one in every five Americans, these challenges must be understood and addressed by providers and payers who wish to continue to serve these populations. Some of these challenges, along with potential strategies to address them, are outlined in the table below.
CONCLUSION: MAKING THE MOST OF MEDICAID MANAGED CARE
Medicaid managed care has the potential to significantly improve access to healthcare and health outcomes for one of the most challenging and complex patient populations—Medicaid members. It may also have the potential to reduce program costs and improve the overall quality of care delivered. However, these goals cannot be achieved unless MCOs are able to create partnerships between providers and payers that can strengthen the delivery of effective, high-quality managed care to the Medicaid population.
The financial and operational challenges for Medicaid MCOs are difficult to overcome, but with proper market insights, patient engagement methodologies, and payer strategies, some key tactics can be used to address the specific issues in each state. Depending on the circumstances, some of these strategies may be more feasible to implement than others, particularly in regard to cost-sensitive strategies such as IT investments. Regardless, employing these tactics can help organizations maximize margins from their Medicaid business under the new MCO model and ultimately deliver better care to a population that has traditionally been underserved.
Footnotes
1. “Expanded Coverage Under the Affordable Care Act: Information for Health Care Professionals,” http://www.medicaid.gov, accessed on October 18, 2015.
5. Vernon K. Smith et al., “Medicaid Reforms to Expand Coverage, Control Costs, and Improve Care: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2015 and 2016,” The Henry J. Kaiser Family Foundation, October 15, 2015


