
Historically, it has been relatively straightforward to distinguish AMCs/primary teaching hospitals from community hospitals. Teaching hospitals serve as hubs of subspecialty care, research, and medical education and treat the highest-acuity and most vulnerable patients. Community hospitals provide convenient access to high-quality care in patients’ local area. However, as the healthcare market continues to evolve, the line that separates academic and community hospitals is quickly blurring.
Intensifying economic and market pressures on AMCs have forced many to diversify their portfolio, expand into new markets, and provide clinical care with little to no academic component. Conversely, increasing physician shortages, the need for differentiation, and technological innovations that enable more complex care to be handled in lower-acuity settings are driving community health systems to train medical residents and conduct their own clinical research. Further contributing to this shift, community health systems are increasingly being called upon to improve the health of the populations they serve, which materially influences their mission and the resources and capabilities required to support these efforts.
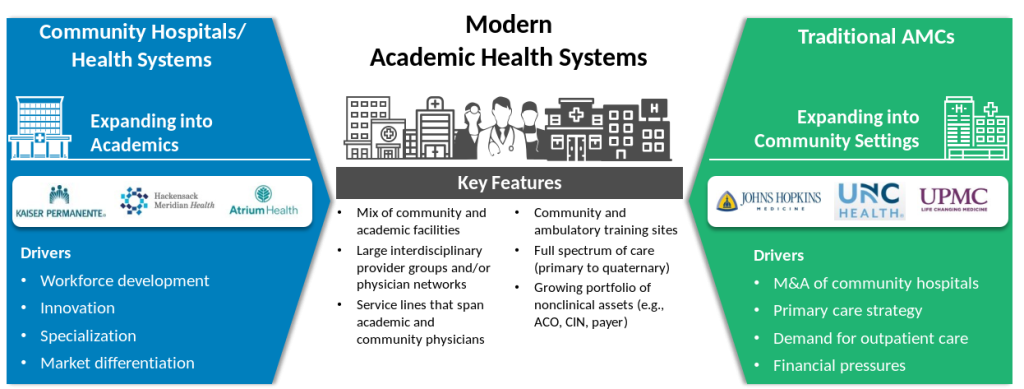
This evolution has resulted in the emergence of modern health systems that span academic and community medicine and provide a full spectrum of care, from primary to quaternary. Exhibit 1 illustrates the driving forces behind this market trend and the key features of the modern academic health system (AHS). This alignment between community and academic organizations has immense benefits for patients, including improved access to clinical services, greater opportunities to participate in clinical trials, and integrated care delivery with potential for better patient outcomes.
This market transformation has slowly but steadily been working across healthcare over the last decade and has left many boards governing an entity that looks entirely different than it did five or 10 years ago. Like the scope of its AHS, the board’s mindset must evolve to ensure continued success. As such, boards should reconsider many facets of governance, including setting strategy, fiduciary oversight, generative thinking, executive oversight, and governance processes and protocols. Key considerations and critical questions for board governance of the evolving (modern) AHS are described in this article.
This article was originally featured in the Governance Institute’s, Academic Health Focus in February 2022.


